how long mandibular nerve heal
The mandibular nerve is a crucial part of the trigeminal nerve, which is the largest cranial nerve in the human body. This nerve supplies sensation to the lower jaw, teeth, chin, and tongue. Injuries or damage to the mandibular nerve can lead to significant pain and discomfort for individuals. Understanding the healing process and the factors influencing it is essential for patients and healthcare professionals alike. In this article, we will delve into the intricacies of the mandibular nerve and explore the expected healing time and recovery process.
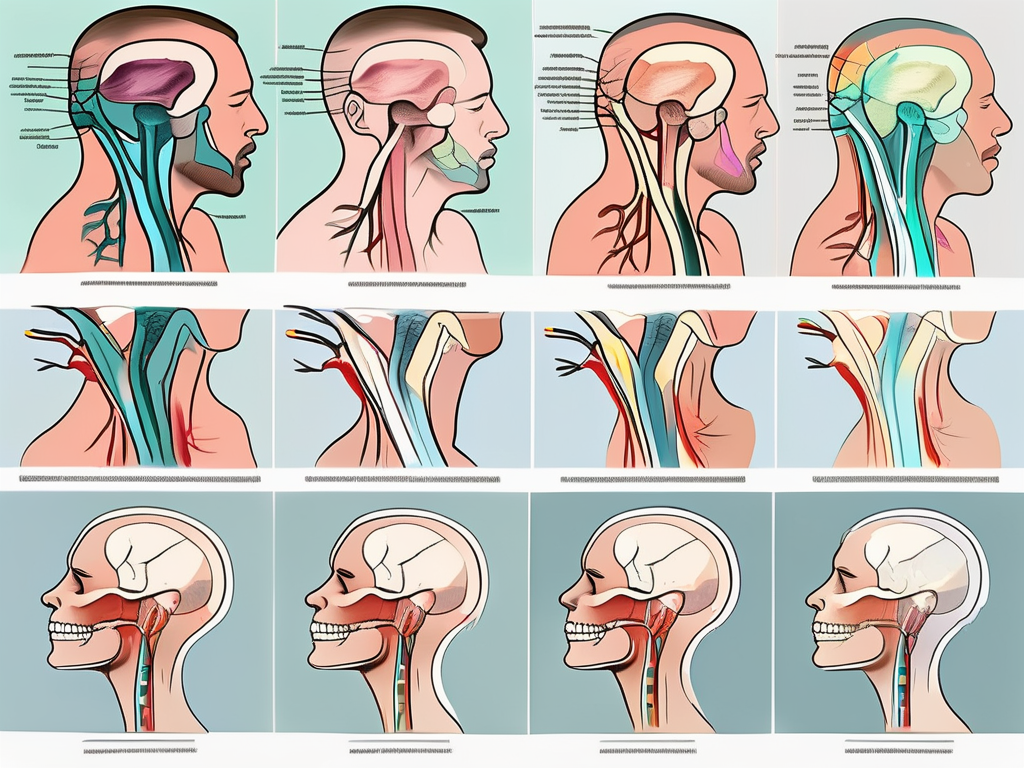
Understanding the Mandibular Nerve
The mandibular nerve, also known as the inferior alveolar nerve, is responsible for transmitting sensory information from the lower part of the face to the brain. It is the largest branch of the trigeminal nerve and has an intricate network of nerve fibers supplying various structures.
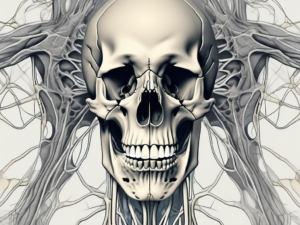
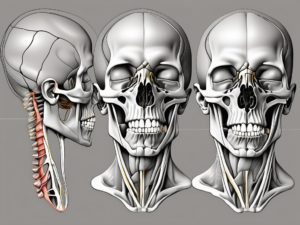
Anatomy of the Mandibular Nerve
The mandibular nerve originates from the trigeminal ganglion, located within the skull. This ganglion is a collection of nerve cell bodies that serve as a relay station for sensory information. From there, the mandibular nerve descends through the skull base, traveling along a complex pathway to reach its destination.
As the mandibular nerve continues its journey, it enters the mandibular foramen, an opening in the lower jawbone. This foramen acts as a gateway, allowing the nerve to extend its reach into the lower face region. Once inside the mandibular foramen, the nerve gives rise to multiple branches, each with a specific function and area of sensory supply.
One of the main branches of the mandibular nerve is the inferior alveolar nerve. This branch provides sensation to the lower teeth and gums. It travels along the mandibular canal, which is a bony tunnel within the lower jawbone that houses the nerve. The inferior alveolar nerve also gives off small branches that innervate the chin and lower lip, contributing to their sensory perception.
Another important branch of the mandibular nerve is the lingual nerve. This nerve supplies sensation to the anterior two-thirds of the tongue, as well as the floor of the mouth. It runs alongside the inferior alveolar nerve within the mandibular canal before branching off to reach its designated areas.
Function of the Mandibular Nerve
The mandibular nerve plays a vital role in chewing, biting, and speaking. It innervates the muscles responsible for these actions, allowing us to perform them with precision and control. Without the mandibular nerve, simple tasks like eating or speaking would become challenging and inefficient.
In addition to its motor function, the mandibular nerve carries sensory information, allowing us to perceive pain, temperature, and touch in the lower face region. This sensory feedback is crucial for our overall well-being and safety. It helps us avoid potential harm by alerting us to dangerous stimuli and allows us to experience the pleasures of touch and taste.
Any damage or disruption to the mandibular nerve can lead to a wide range of symptoms and functional impairments. Nerve injuries can occur due to trauma, infection, or certain medical conditions. Common symptoms of mandibular nerve damage include numbness or tingling in the lower face, pain or sensitivity in the teeth or gums, difficulty chewing or speaking, and altered sensation in the tongue.
Understanding the anatomy and function of the mandibular nerve is essential for healthcare professionals, particularly dentists and oral surgeons. It enables them to diagnose and treat various conditions affecting this nerve, ensuring optimal oral health and overall well-being for their patients.
Causes of Mandibular Nerve Damage
Mandibular nerve damage can occur due to various factors, ranging from dental procedures to traumatic injuries. Understanding the potential causes is crucial for prevention and timely intervention.
Dental Procedures and Risks
During certain dental procedures such as wisdom tooth extraction, placement of dental implants, or administration of anesthesia, there is a risk of unintentionally damaging the mandibular nerve. This can lead to temporary or permanent nerve dysfunction, with associated symptoms.
When it comes to wisdom tooth extraction, the close proximity of the mandibular nerve to the wisdom tooth roots increases the chances of accidental nerve injury. Dentists must exercise caution and skill during the extraction process to minimize the risk.
In the case of dental implant placement, the mandibular nerve can be damaged if the implant is inserted too close to the nerve or if the drilling process causes trauma to the nerve. Dentists rely on careful planning, including the use of radiographs and computer-guided surgery, to avoid such complications.
Administering anesthesia is another potential source of mandibular nerve damage. Anesthesia injections, if not performed correctly, can lead to nerve injury. Dentists must be well-trained in the proper techniques to ensure patient safety.
Trauma and Injuries
Accidental trauma to the face, jaw, or lower jawbone can also result in mandibular nerve damage. Fractures, dislocations, or direct impact on the nerve can compromise its integrity and disrupt the transmission of sensory signals.
Motor vehicle accidents, sports injuries, or falls can all cause significant trauma to the face and jaw, potentially leading to mandibular nerve damage. The force of impact can directly injure the nerve or cause fractures that impinge upon it.
In some cases, mandibular nerve damage may occur as a result of surgical procedures to repair facial fractures. While these surgeries aim to restore the structural integrity of the face, they carry a risk of nerve injury due to the delicate nature of the nerves in the area.
It is important to note that the severity of mandibular nerve damage can vary depending on the extent and nature of the trauma. Mild cases may resolve on their own with time, while more severe cases may require surgical intervention or ongoing management to alleviate symptoms and restore normal nerve function.
Symptoms of Mandibular Nerve Damage
Mandibular nerve damage can result in a range of physical and psychological symptoms. Recognizing these symptoms is crucial for early detection and appropriate management.
Mandibular nerve damage is a condition that can have a significant impact on a person’s daily life. The symptoms can vary from person to person, but there are some common physical and psychological effects that individuals may experience.
Physical Symptoms
Patients with mandibular nerve damage may experience numbness or a tingling sensation in the lower jaw, teeth, chin, or tongue. This sensation can be persistent or intermittent, and it can range from mild to severe. The affected areas may also feel sensitive to touch or pressure.
In addition to the sensory symptoms, individuals with mandibular nerve damage may develop difficulty in chewing, biting, or speaking. This can make it challenging to eat certain foods or communicate effectively. They may also experience discomfort or pain in the affected areas, which can range from a dull ache to sharp, shooting pains.
The physical symptoms of mandibular nerve damage can have a significant impact on a person’s ability to carry out daily activities. Simple tasks like eating, talking, or even smiling can become challenging and painful.
Emotional and Psychological Impact
Living with mandibular nerve damage can have emotional and psychological implications for individuals. The chronic pain and functional limitations associated with this condition can lead to feelings of frustration, helplessness, and even isolation.
Individuals with mandibular nerve damage may also experience changes in their appearance, such as facial asymmetry or drooping of the lower lip. These changes can affect a person’s self-esteem and body image, leading to feelings of self-consciousness and social withdrawal.
The emotional and psychological impact of mandibular nerve damage can extend beyond the physical symptoms. Anxiety and depression are common among individuals with chronic pain conditions, and mandibular nerve damage is no exception. The constant discomfort and limitations can contribute to feelings of sadness, hopelessness, and overall reduced quality of life.
It is important for individuals with mandibular nerve damage to seek appropriate medical care and support. A multidisciplinary approach, involving healthcare professionals such as neurologists, dentists, and psychologists, can help manage the physical and psychological aspects of this condition.
Diagnosis of Mandibular Nerve Damage
Accurate diagnosis is critical for determining the extent of mandibular nerve damage and formulating an appropriate treatment plan. Healthcare professionals utilize a combination of medical history, physical examination, and diagnostic tests for evaluation.
When it comes to diagnosing mandibular nerve damage, healthcare providers understand the importance of gathering a comprehensive medical history. During the medical history assessment, healthcare providers inquire about the onset, duration, and progression of symptoms. They carefully listen to the patient’s description of their symptoms, paying close attention to any factors that may have triggered or worsened the condition. By understanding the timeline of the symptoms, healthcare providers can gain valuable insights into the potential causes and severity of the nerve damage.
In addition to the medical history assessment, healthcare providers perform a thorough physical examination to further evaluate the mandibular nerve damage. They meticulously assess sensory function, muscle strength, and coordination in the affected areas. By conducting sensory tests, healthcare providers can determine if there is any loss of sensation or abnormal sensations in the mandibular nerve distribution. Muscle strength and coordination tests help healthcare providers assess the impact of the nerve damage on the patient’s ability to move their jaw and perform daily activities.
Imaging and Other Diagnostic Tests
While medical history and physical examination provide valuable information, healthcare providers often rely on diagnostic imaging techniques to visualize the mandibular nerve and detect any structural abnormalities or injuries. X-rays, computed tomography (CT), or magnetic resonance imaging (MRI) may be employed to obtain detailed images of the mandibular nerve and surrounding structures. These imaging techniques allow healthcare providers to assess the anatomical integrity of the nerve and identify any potential causes of the damage, such as fractures, tumors, or compression.
In addition to imaging, healthcare providers may also utilize specialized tests to assess the function and integrity of the mandibular nerve. Electromyography (EMG) is a diagnostic test that measures the electrical activity of muscles. By inserting small needles into the muscles surrounding the mandibular nerve, healthcare providers can evaluate the nerve’s ability to transmit electrical signals and assess the overall muscle function. Nerve conduction studies (NCS) are another diagnostic test that measures the speed and strength of electrical signals as they travel along the mandibular nerve. These tests provide valuable information about the nerve’s functionality and can help healthcare providers determine the extent of the damage.
Overall, the diagnosis of mandibular nerve damage involves a comprehensive approach that combines medical history assessment, physical examination, and diagnostic tests. By gathering as much information as possible, healthcare providers can accurately assess the extent of the damage and develop an appropriate treatment plan tailored to the individual needs of the patient.
Treatment Options for Mandibular Nerve Damage
The treatment of mandibular nerve damage depends on the underlying cause, severity of symptoms, and the individual’s overall health. A comprehensive approach may involve medications, non-surgical interventions, or surgical procedures.
Mandibular nerve damage can occur as a result of various factors, including trauma, infection, or underlying medical conditions such as trigeminal neuralgia or temporomandibular joint disorder (TMJ). The severity of the damage can range from mild discomfort to debilitating pain and loss of function.
When it comes to treating mandibular nerve damage, healthcare professionals take into consideration the specific needs and circumstances of each individual. This personalized approach ensures that the most appropriate treatment plan is developed.
Medications and Non-Surgical Treatments
In certain cases, medications such as analgesics, anti-inflammatory drugs, or nerve stabilizers may be prescribed to alleviate pain and manage associated symptoms. These medications work by targeting the underlying causes of nerve damage, reducing inflammation, and providing relief from pain.
Additionally, non-surgical treatments can play a crucial role in the management of mandibular nerve damage. Physical therapy, for example, can help improve muscle strength and coordination, which can alleviate symptoms and enhance overall function. Therapists may employ a range of exercises and techniques tailored to the individual’s specific needs.
Furthermore, complementary therapies such as acupuncture or chiropractic care may be considered as part of the treatment plan. These alternative approaches aim to stimulate the body’s natural healing mechanisms and promote overall well-being.
Surgical Interventions
In more severe cases of mandibular nerve damage, surgical intervention may be necessary. Nerve repair or reconstruction procedures can be performed to restore the integrity and function of the damaged nerve.
During nerve repair surgery, the damaged section of the nerve is carefully identified and repaired using microsurgical techniques. This delicate procedure aims to reconnect the nerve fibers, allowing for the restoration of normal nerve function.
In cases where the nerve damage is extensive or irreparable, nerve grafting may be considered. This procedure involves taking a healthy nerve from another part of the body and using it to bridge the gap in the damaged nerve. The graft serves as a conduit for nerve regeneration, facilitating the restoration of function.
It is important to note that the success of surgical interventions for mandibular nerve damage depends on various factors, including the extent of the damage, the individual’s overall health, and their ability to undergo and recover from surgery. Additionally, outcomes may vary from person to person, and it is crucial to have realistic expectations and open communication with the healthcare team.
In conclusion, the treatment options for mandibular nerve damage are diverse and tailored to the individual’s specific needs. From medications and non-surgical interventions to surgical procedures, healthcare professionals strive to provide comprehensive care that aims to alleviate pain, restore function, and improve overall quality of life.
Recovery and Healing Process of the Mandibular Nerve
The recovery and healing process of the mandibular nerve is a complex phenomenon influenced by multiple factors. Understanding the expected healing time and the variables affecting it can provide insights into the journey of recovery.
Expected Healing Time
The duration of mandibular nerve healing can vary considerably depending on the severity of the damage, individual factors, and the chosen treatment approach. While some cases may resolve within weeks or months, others may require a longer healing period.
Factors Affecting Healing
Several factors can influence the healing process of the mandibular nerve. Age, overall health, presence of underlying medical conditions, adherence to treatment, and lifestyle modifications can all play a role in the recovery timeline. It is crucial for individuals to closely follow their healthcare provider’s recommendations and monitor their progress accordingly.
Prevention and Management of Mandibular Nerve Damage
Preventing mandibular nerve damage is always preferable to treatment. Dental professionals should exercise caution during procedures that pose a risk of nerve injury. It is essential for patients to communicate any concerns or symptoms to their healthcare provider promptly.
Precautions during Dental Procedures
Dental professionals should carefully assess the anatomical variations and thoroughly examine radiographic images before performing procedures near the mandibular nerve. Employing proper techniques, using appropriate instruments, and being attentive to patient feedback can minimize the risk of nerve damage.
Lifestyle Changes and Home Remedies
After a mandibular nerve injury, individuals can make certain lifestyle changes and utilize home remedies to support the healing process. These can include following a well-balanced diet, practicing stress management techniques, maintaining oral hygiene, and avoiding habits that can exert excessive pressure on the nerve.
Future Research and Developments in Mandibular Nerve Healing
Advancements in medical science continue to drive research into new treatments and interventions for mandibular nerve healing. The quest for nerve regeneration techniques and innovative therapies holds promising potential for the future.
Advances in Medical Treatments
Ongoing research focuses on developing pharmacological agents, growth factors, and biological therapies that can enhance nerve regeneration and support healing in cases of mandibular nerve damage.
Potential Breakthroughs in Nerve Regeneration
Emerging technologies, such as tissue engineering, stem cell therapy, and nerve grafting techniques, offer hope for achieving successful nerve repair and regeneration. These exciting breakthroughs may revolutionize the management of mandibular nerve damage in the years to come.
In conclusion, the healing process of the mandibular nerve is unique to each individual and influenced by various factors. Recognizing the symptoms, seeking timely medical evaluation, and following the recommended treatment approach are crucial for optimizing recovery. It is imperative to consult with a healthcare professional for appropriate diagnosis and management of mandibular nerve damage. With ongoing advancements in medical science, the future holds promise for more effective treatments and improved outcomes.