how to avoid marginal mandibular nerve injury
The marginal mandibular nerve is a crucial component of the facial nerve network. This nerve carries motor signals from the brain to the muscles responsible for controlling important facial expressions, such as smiling and frowning. Unfortunately, injuries to the marginal mandibular nerve can occur, causing functional impairment and aesthetic limitations.
Understanding the Marginal Mandibular Nerve
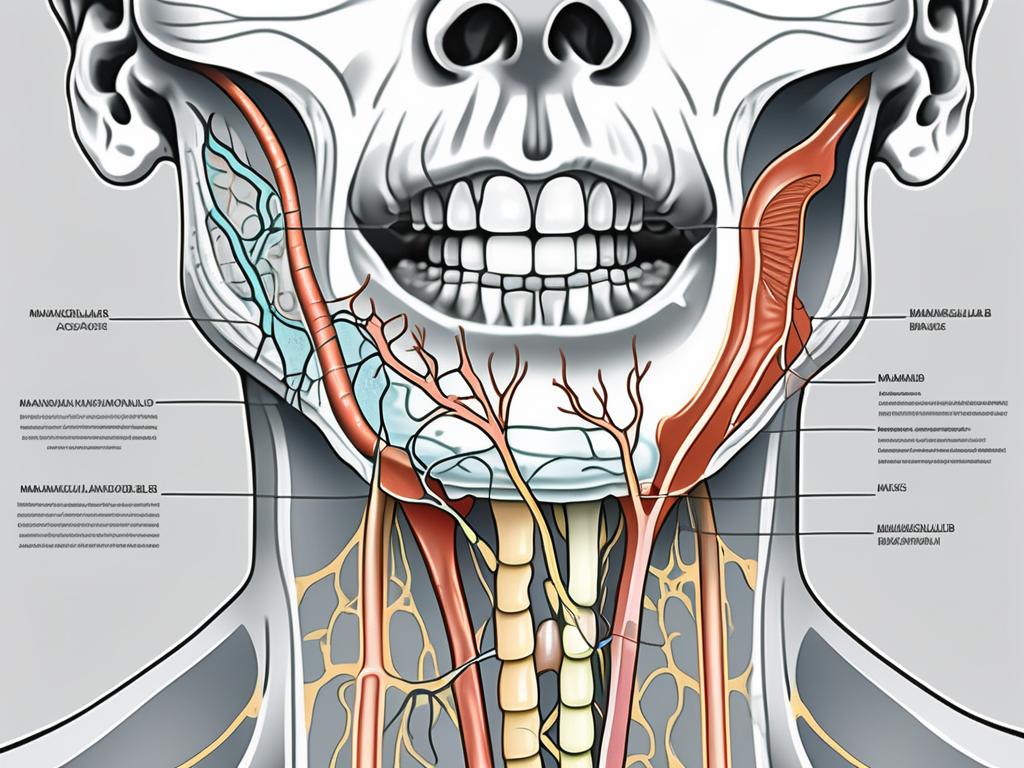
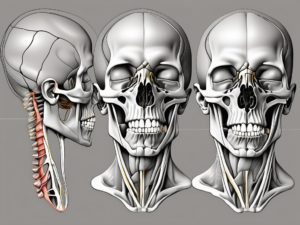
In order to effectively prevent and address marginal mandibular nerve injury, it is important to have a comprehensive understanding of the nerve’s anatomy and function. The marginal mandibular nerve is a branch of the facial nerve, specifically originating from the mandibular division. It travels in a downward direction, running along the jawline and innervating the muscles of the lower lip and chin.
Anatomy of the Marginal Mandibular Nerve
The marginal mandibular nerve is located superficially, underneath the skin and subcutaneous tissue. It roughly follows the contour of the jaw bone, maintaining a relatively consistent position. Awareness of its anatomical course is crucial for healthcare professionals performing surgical procedures in the area.
As the nerve descends along the jawline, it courses through a complex network of connective tissue and blood vessels. This intricate pathway provides protection and support for the nerve, ensuring its proper functioning. The nerve’s proximity to the surface of the skin also allows for easier identification during surgical procedures.
Within the connective tissue, the marginal mandibular nerve is surrounded by a delicate sheath known as the epineurium. This protective layer helps to insulate the nerve fibers and maintain their structural integrity. It also serves as a barrier against potential sources of damage, such as compression or trauma.
Function of the Marginal Mandibular Nerve
The marginal mandibular nerve plays a vital role in the functionality of the lower face. It innervates the depressor anguli oris muscle, allowing for the downward movement of the lip. This muscle is responsible for various facial expressions, such as frowning or pouting.
In addition to its role in lip movement, the marginal mandibular nerve also supplies the mentalis muscle. This muscle is located in the chin region and contributes to chin movement and expression. It plays a crucial role in actions such as chin protrusion, aiding in speech production and facial gestures.
Furthermore, the marginal mandibular nerve is involved in the coordination of other facial muscles, including the platysma muscle. The platysma muscle extends from the lower jaw to the collarbone and is responsible for various movements of the neck and lower face. The marginal mandibular nerve’s innervation of this muscle allows for coordinated movements of the lower face and neck, contributing to overall facial expression and motor function.
Given its extensive role in facial expression and motor function, the integrity of the marginal mandibular nerve is essential for preserving natural facial expressions and overall facial symmetry. Damage or injury to the nerve can result in various functional impairments, including weakness or paralysis of the lower lip and chin, as well as asymmetry of facial movements.
Understanding the anatomy and function of the marginal mandibular nerve is crucial for healthcare professionals involved in surgical procedures in the lower face and neck region. By having a comprehensive knowledge of the nerve’s course, protective mechanisms, and functional implications, healthcare providers can minimize the risk of nerve injury and ensure optimal patient outcomes.
Risks of Marginal Mandibular Nerve Injury
While the marginal mandibular nerve is generally well-protected, certain factors can increase the risk of nerve injury. It is crucial for healthcare professionals to be aware of these risks and take appropriate preventative measures.
The marginal mandibular nerve, also known as the lower branch of the facial nerve, is responsible for innervating the muscles of the lower lip and chin. This nerve plays a vital role in facial expression, speech, and eating. Any damage to this nerve can have significant consequences for the patient.
Common Causes of Injury
One of the primary causes of marginal mandibular nerve injury is surgical procedures involving the lower face and neck region. Surgeries such as facelifts, neck lift procedures, and certain dental procedures carry a risk of nerve damage, particularly if proper precautions are not taken.
During facelift surgeries, for example, the surgeon may need to manipulate the tissues around the lower face and neck to achieve the desired aesthetic outcome. However, if the surgeon is not careful, they may inadvertently injure the marginal mandibular nerve, leading to potential complications.
In dental procedures, such as wisdom tooth extraction or dental implant placement, the proximity of the nerve to the surgical site increases the risk of accidental injury. Dentists must exercise caution and employ techniques to minimize the chances of nerve damage.
Potential Complications and Consequences
Marginal mandibular nerve injury can lead to a range of complications and consequences. Loss of muscle function in the lower lip and chin can result in asymmetry and difficulty with speech, eating, and facial expressions. Patients may find it challenging to pronounce certain sounds or words, leading to communication difficulties.
In addition to functional impairments, patients may also experience psychological distress due to the visible changes in their facial appearance. Asymmetry and drooping of the lower lip can significantly impact one’s self-esteem and confidence.
Some patients may also report sensory changes in the affected area. Numbness or tingling sensations may be present, further adding to the discomfort and potential functional limitations.
It is essential for healthcare professionals to be vigilant in preventing and promptly addressing nerve injuries to minimize the potential negative outcomes. Proper preoperative planning, meticulous surgical technique, and postoperative monitoring can significantly reduce the risk of marginal mandibular nerve injury.
Furthermore, patient education plays a crucial role in managing expectations and ensuring that individuals are aware of the potential risks associated with surgical procedures involving the lower face and neck region. By providing comprehensive information and addressing any concerns, healthcare professionals can empower patients to make informed decisions regarding their treatment options.
Prevention Strategies for Marginal Mandibular Nerve Injury
Healthcare professionals must implement effective prevention strategies to minimize the occurrence of marginal mandibular nerve injuries. By adhering to best practices and utilizing non-surgical prevention methods, the risk of nerve injury can be significantly reduced.
Best Practices in Surgical Procedures
During surgical procedures involving the lower face and neck, healthcare professionals should exercise extra caution to protect the marginal mandibular nerve. Techniques such as meticulous dissection, gentle tissue handling, and visualization aids, such as nerve monitoring devices, can greatly reduce the risk of inadvertent nerve damage.
When performing dissection, healthcare professionals should prioritize meticulousness. By carefully separating tissues and structures, they can minimize the risk of damaging the marginal mandibular nerve. Additionally, gentle tissue handling is crucial to prevent unnecessary trauma to the nerve. Healthcare professionals should handle tissues with care, using delicate instruments and avoiding excessive force.
Furthermore, the use of visualization aids, such as nerve monitoring devices, can provide real-time feedback on the proximity and integrity of the marginal mandibular nerve. These devices can help healthcare professionals identify potential risks and make adjustments during the surgical procedure to avoid nerve injury.
Non-surgical Prevention Methods
In non-surgical settings, healthcare professionals should ensure proper communication with patients to gather relevant medical history and identify any pre-existing conditions that may increase the risk of nerve injury. Patient education is paramount, emphasizing the importance of reporting any unusual symptoms or sensations. Periodic follow-ups to monitor nerve function can also be beneficial in detecting potential issues early.
When interacting with patients, healthcare professionals should take the time to gather a comprehensive medical history. This information can help identify any pre-existing conditions, such as diabetes or peripheral neuropathy, that may make the marginal mandibular nerve more susceptible to injury. By understanding the patient’s medical background, healthcare professionals can tailor their approach and take additional precautions if necessary.
Patient education plays a crucial role in preventing marginal mandibular nerve injuries. Healthcare professionals should educate patients about the potential risks and symptoms associated with nerve injury. Patients should be encouraged to report any unusual sensations, such as numbness, tingling, or weakness in the lower face and neck region. By promptly addressing these symptoms, healthcare professionals can intervene early and prevent further nerve damage.
Additionally, periodic follow-ups can be an effective preventive measure. By monitoring the patient’s nerve function over time, healthcare professionals can detect any changes or abnormalities. Regular assessments can help identify potential issues before they progress, allowing for timely intervention and minimizing the risk of long-term nerve damage.
Recognizing the Symptoms of Marginal Mandibular Nerve Injury
Early recognition and prompt intervention are crucial when it comes to marginal mandibular nerve injuries. Healthcare professionals play a vital role in identifying and assessing potential cases.
Marginal mandibular nerve injury, also known as marginal mandibular branch palsy, occurs when there is damage or compression to the marginal mandibular nerve. This nerve is a branch of the facial nerve and is responsible for controlling the muscles of the lower lip and chin. When injured, it can lead to a range of symptoms that can significantly impact a person’s facial movement and functionality.
Early Signs of Injury
Early signs of marginal mandibular nerve injury may include weakness or drooping of the lower lip on the affected side, difficulty with lip control, and an asymmetrical smile. These symptoms can be distressing for patients, as they may affect their ability to speak, eat, and perform daily activities.
In addition to the physical symptoms, patients may also experience pain or discomfort in the region surrounding the nerve. This pain can vary in intensity and may be exacerbated by activities that require facial muscle movement, such as talking or chewing.
Progression of Symptoms
If left untreated, the symptoms of marginal mandibular nerve injury can worsen over time. The progression of symptoms can vary from person to person, but it is essential for healthcare professionals to be aware of the potential for deterioration.
As the injury progresses, patients may experience further impairments in facial movement and functionality. This can include increased weakness or paralysis of the lower lip, difficulty in closing the affected eye, and changes in the appearance of the chin and lower face. These changes can have a significant impact on a person’s self-esteem and overall quality of life.
Therefore, it is crucial for healthcare professionals to monitor patients closely and intervene promptly if any signs of progression are observed. Early intervention can help prevent further damage to the nerve and improve the chances of a successful recovery.
In conclusion, recognizing the symptoms of marginal mandibular nerve injury is essential for early intervention and optimal patient outcomes. Healthcare professionals should be vigilant in assessing patients for signs of nerve injury and provide appropriate care and support to minimize the impact on their daily lives.
Treatment Options for Marginal Mandibular Nerve Injury
If a marginal mandibular nerve injury is suspected or confirmed, healthcare professionals can implement various treatment options to address the issue and facilitate recovery.
When a patient presents with symptoms that suggest a marginal mandibular nerve injury, it is crucial for healthcare professionals to respond promptly and effectively. Immediate communication with the patient is essential to gather a detailed medical history and understand the extent of the injury. This information will help guide the treatment plan and determine the appropriate course of action.
Referral to specialists, such as a facial plastic surgeon or neurologist, might be necessary to further evaluate the injury and develop a comprehensive treatment strategy. These experts have the knowledge and expertise to assess the severity of the nerve damage and recommend the most suitable interventions.
Treatment options for marginal mandibular nerve injuries can vary depending on the specific circumstances and severity of the injury. In less severe cases, conservative approaches like physical therapy and medication may be sufficient to promote healing and restore normal nerve function.
Physical therapy plays a crucial role in the management and rehabilitation of marginal mandibular nerve injuries. Skilled therapists can design personalized exercise programs that target the affected muscles and stimulate nerve regeneration. These exercises may include facial muscle strengthening exercises, range of motion exercises, and sensory re-education techniques.
In more severe cases, surgical intervention may be necessary to repair the damaged nerve. Surgical procedures can involve nerve grafting, nerve transfer, or direct nerve repair, depending on the specific circumstances of the injury. These procedures aim to restore nerve continuity and facilitate functional recovery.
After the initial treatment, long-term management and rehabilitation are vital for optimal recovery. Regular follow-ups with healthcare professionals will allow for ongoing monitoring and adjustment of treatment plans as needed. These follow-up appointments provide an opportunity to assess the progress of nerve regeneration, address any complications that may arise, and modify the treatment approach accordingly.
Additionally, healthcare professionals may recommend complementary therapies to enhance the recovery process. These may include acupuncture, electrical stimulation, or massage therapy, which can help improve blood circulation, reduce inflammation, and promote nerve regeneration.
It is important for patients to actively participate in their own recovery by following the prescribed treatment plan and adhering to any lifestyle modifications recommended by healthcare professionals. This may include avoiding activities that could potentially aggravate the injury, practicing good oral hygiene, and adopting stress-reduction techniques to promote overall well-being.
In conclusion, the treatment options for marginal mandibular nerve injuries are diverse and depend on the severity of the injury. Prompt communication with the patient, referral to specialists, and a comprehensive treatment plan that may include physical therapy, medication, or surgical intervention are crucial for optimal recovery. Long-term management and rehabilitation, along with regular follow-ups, are essential to monitor progress and adjust treatment plans as needed. By actively participating in their own recovery, patients can maximize the chances of restoring normal nerve function and improving their overall quality of life.
The Role of Healthcare Professionals in Avoiding Injury
Healthcare professionals, specifically surgeons and dentists, have a significant responsibility in avoiding marginal mandibular nerve injury. By adhering to proper protocols and effectively communicating with patients, they can minimize the occurrence of such injuries.
When it comes to the responsibilities of surgeons and dentists, patient safety should always be their top priority. They must take appropriate precautions during procedures that carry a risk of marginal mandibular nerve injury. This includes meticulous planning, where they carefully assess the patient’s medical history, conduct thorough examinations, and consider any potential risk factors that may increase the likelihood of nerve injury.
Moreover, upholding surgical principles that prioritize nerve preservation is of utmost importance. Surgeons and dentists must be well-versed in the anatomy of the marginal mandibular nerve and exercise precision and caution during procedures to avoid any inadvertent damage to this delicate nerve.
Responsibilities of Surgeons and Dentists
Surgeons and dentists should prioritize patient safety and take appropriate precautions during procedures that carry a risk of marginal mandibular nerve injury. This includes, but is not limited to, meticulous planning, proper patient assessment, and upholding surgical principles that prioritize nerve preservation.
Additionally, healthcare professionals should stay updated with the latest advancements in surgical techniques and technologies that can help minimize the risk of nerve injury. By continuously expanding their knowledge and skills, they can provide the best possible care to their patients and reduce the chances of complications.
Collaboration among healthcare professionals is also crucial in avoiding nerve injuries. Surgeons and dentists should work closely with an interdisciplinary team, including anesthesiologists, nurses, and other specialists, to ensure comprehensive patient care. By sharing information, expertise, and insights, they can collectively develop strategies to prevent nerve injuries and enhance patient outcomes.
Patient Education and Communication
Healthcare professionals have a duty to educate patients about the potential risks associated with procedures involving the marginal mandibular nerve. Providing clear and accurate information about potential complications and the importance of reporting unusual symptoms can empower patients to actively participate in their own care and seek timely medical attention if necessary.
During the pre-operative consultation, surgeons and dentists should take the time to explain the procedure in detail, including the specific risks and potential complications related to the marginal mandibular nerve. They should ensure that patients fully understand the importance of following post-operative instructions and reporting any unexpected symptoms, such as numbness, tingling, or weakness in the lower face or neck region.
Furthermore, healthcare professionals should encourage open communication with their patients. They should create a safe and non-judgmental environment where patients feel comfortable expressing their concerns and asking questions. By fostering a strong patient-provider relationship based on trust and mutual respect, healthcare professionals can effectively address any anxieties or uncertainties that patients may have, ultimately enhancing patient satisfaction and promoting better overall outcomes.
Conclusion
Preventing and addressing marginal mandibular nerve injury requires a collective effort from healthcare professionals and patients alike. By prioritizing anatomical knowledge, implementing preventative strategies, and promptly recognizing and treating any injuries, the risk of nerve damage can be significantly reduced. However, it is essential for patients to consult with their healthcare providers for personalized advice and guidance regarding their specific circumstances.