how to ease mandibular nerve pain
Mandibular nerve pain, also known as trigeminal neuralgia, can be a debilitating condition that affects the trigeminal nerve, the largest cranial nerve responsible for innervating the face. This article aims to provide a comprehensive understanding of mandibular nerve pain, its symptoms, diagnosis, treatment options, and prevention methods. It is important to note that while this article offers valuable information, it is not a substitute for professional medical advice. If you are experiencing mandibular nerve pain, it is crucial to consult with a qualified healthcare provider for proper diagnosis and treatment options.
Understanding Mandibular Nerve Pain
Mandibular nerve pain, also known as trigeminal neuralgia or TN, is characterized by severe, intermittent, and lancinating facial pain. The mandibular nerve, which is the third branch of the trigeminal nerve, supplies sensation to the lower jaw, lower lip, and chin area. When this nerve becomes irritated or compressed, it can result in excruciating pain.
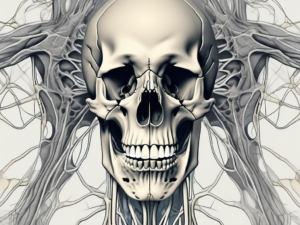
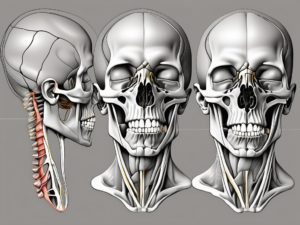
Anatomy of the Mandibular Nerve
The mandibular nerve consists of sensory fibers that originate from the trigeminal ganglion, located within the skull. It branches out into multiple divisions, including the buccal, lingual, and inferior alveolar nerves. These branches supply innervation to various structures in the face, including the jaw, teeth, and gums.
The buccal nerve provides sensation to the cheek and the buccal mucosa, which lines the inside of the cheek. It plays a crucial role in the ability to chew and speak properly. The lingual nerve, on the other hand, supplies sensation to the tongue, including the taste buds. It allows us to enjoy the flavors of our favorite foods. Lastly, the inferior alveolar nerve provides sensation to the lower teeth and gums, allowing us to perceive pressure, temperature, and pain in that area.
Common Causes of Mandibular Nerve Pain
Mandibular nerve pain can have various underlying causes, including:
- Compression of the nerve due to blood vessels: Sometimes, blood vessels can exert pressure on the mandibular nerve, leading to pain and discomfort. This compression can occur due to anatomical variations or as a result of certain medical conditions.
- Nerve damage from trauma or surgery: Injuries to the face or jaw, such as fractures or surgical procedures, can potentially damage the mandibular nerve. This can result in persistent pain and altered sensation in the affected area.
- Dental conditions, such as abscesses or impacted molars: Dental infections, such as abscesses, can spread to the surrounding tissues and affect the mandibular nerve. Additionally, impacted molars, which are teeth that fail to fully emerge from the gums, can put pressure on the nerve, causing pain.
- Multiple sclerosis or other neurological disorders: Certain neurological conditions, including multiple sclerosis, can affect the function of the mandibular nerve. This can lead to pain and other sensory abnormalities in the lower face.
Identifying the exact cause of mandibular nerve pain is crucial for determining the most appropriate treatment approach. Therefore, a comprehensive evaluation by a healthcare professional is necessary. They will take into account the patient’s medical history, perform a physical examination, and may order additional tests, such as imaging studies or nerve conduction tests, to aid in the diagnosis.
Symptoms Associated with Mandibular Nerve Pain
The hallmark symptom of mandibular nerve pain is intense facial pain, which can be triggered by everyday activities such as chewing, talking, or even light touch. However, there are other symptoms associated with this condition that can significantly impact an individual’s quality of life.
Mandibular nerve pain, also known as trigeminal neuralgia, is a neurological disorder that affects the trigeminal nerve, which is responsible for transmitting sensory information from the face to the brain. When this nerve becomes irritated or damaged, it can result in excruciating pain that can be debilitating.
In addition to severe facial pain, individuals with mandibular nerve pain may experience a range of physical symptoms. Facial muscle spasms are a common occurrence, causing involuntary contractions that can further intensify the pain. Tingling or numbing sensations in the affected area are also reported, adding to the discomfort and distress.
Interestingly, some individuals with mandibular nerve pain notice an increase in pain during cold or windy weather. The exact reason behind this phenomenon is not fully understood, but it is believed that the changes in temperature and air pressure may irritate the nerve, leading to heightened pain sensitivity.
Another characteristic of mandibular nerve pain is the occurrence of abrupt episodes of pain, often described as electric shocks or stabbing sensations. These episodes can last from a few seconds to several minutes and can be triggered by seemingly innocuous actions such as brushing the teeth or touching the face.
It is important to note that the severity and frequency of symptoms can vary from person to person. Some individuals may experience occasional mild episodes, while others may endure constant and severe pain that significantly impacts their daily lives.
Emotional and Psychological Effects
Living with chronic facial pain can take a toll on an individual’s emotional well-being. The constant fear of pain episodes and the limitations it imposes on daily activities can lead to anxiety, depression, and social isolation.
The emotional impact of mandibular nerve pain should not be underestimated. The relentless pain can cause individuals to feel helpless, frustrated, and overwhelmed. It can disrupt sleep patterns, making it difficult to get adequate rest and exacerbating feelings of fatigue and irritability.
Furthermore, the unpredictable nature of the pain can make individuals hesitant to engage in social activities or even leave their homes. The fear of experiencing a pain episode in public can lead to social withdrawal and isolation, which can further contribute to feelings of loneliness and depression.
Seeking support from loved ones, mental health professionals, or support groups can help individuals cope with these emotional and psychological challenges. Connecting with others who are going through similar experiences can provide a sense of validation, understanding, and encouragement.
Additionally, exploring relaxation techniques, such as deep breathing exercises, meditation, or yoga, can help individuals manage stress and reduce the impact of emotional distress on their overall well-being.
In conclusion, mandibular nerve pain is a debilitating condition characterized by intense facial pain and a range of physical symptoms. It can have profound emotional and psychological effects, impacting an individual’s quality of life. Understanding and addressing these effects is crucial for comprehensive management and support for individuals living with mandibular nerve pain.
Diagnosis of Mandibular Nerve Pain
Proper diagnosis of mandibular nerve pain requires a thorough evaluation of the individual’s medical history, physical examination, and, in some cases, additional imaging or laboratory tests.
Medical History and Physical Examination
A healthcare professional will review the individual’s medical history, paying close attention to the nature of their pain, triggers, and associated symptoms. This comprehensive assessment helps to identify any potential underlying causes or contributing factors to the mandibular nerve pain.
During the physical examination, the healthcare professional will conduct a detailed assessment of the affected areas. This may involve palpating the jaw, neck, and facial muscles to identify any areas of tenderness or muscle spasms. They will also assess the function and sensitivity of the affected areas, evaluating the individual’s ability to open and close their mouth, chew, and speak without discomfort.
In addition to the examination of the jaw and facial region, the healthcare professional may also examine the individual’s teeth and gums. This is important as dental problems, such as tooth decay or gum disease, can sometimes cause referred pain to the mandibular nerve.
Imaging and Laboratory Tests
In some cases, imaging tests such as magnetic resonance imaging (MRI) or computed tomography (CT) scans may be ordered to rule out other underlying causes of facial pain, such as tumors or structural abnormalities. These imaging tests provide detailed images of the bones, soft tissues, and nerves in the jaw and face, helping to identify any potential sources of nerve compression or damage.
Additionally, blood tests may be performed to evaluate for any signs of inflammation or infection. Elevated levels of certain markers in the blood can indicate the presence of an underlying condition, such as an autoimmune disorder or an infection, which may be contributing to the mandibular nerve pain.
Furthermore, if the healthcare professional suspects that the mandibular nerve pain is related to a specific dental issue, they may refer the individual to a dentist for further evaluation. The dentist may perform dental X-rays or other dental imaging tests to assess the health of the teeth, gums, and surrounding structures.
Overall, the diagnosis of mandibular nerve pain involves a comprehensive approach, combining the individual’s medical history, physical examination, and, if necessary, additional imaging or laboratory tests. This thorough evaluation helps to accurately identify the underlying cause of the pain, allowing for appropriate treatment and management strategies to be implemented.
Non-Surgical Treatment Options
The management of mandibular nerve pain typically begins with non-surgical treatment options. These aim to alleviate pain and improve the individual’s quality of life. The specific treatment plan may vary depending on the underlying cause and the severity of symptoms.
When it comes to managing mandibular nerve pain, there are several non-surgical treatment options available. These options range from medications to physical therapy techniques and even alternative therapies. Each of these approaches has its own benefits and considerations, and the choice of treatment depends on the individual’s specific needs and preferences.
Medications for Mandibular Nerve Pain
Pain medications, including anticonvulsants and tricyclic antidepressants, are often prescribed to help control the facial pain associated with mandibular nerve pain. Anticonvulsants work by stabilizing the electrical activity in the nerves, reducing their sensitivity to pain signals. Tricyclic antidepressants, on the other hand, can help regulate the levels of certain chemicals in the brain, which can alleviate pain and improve mood.
It is important to note that while medications can be effective in managing mandibular nerve pain, they may also have potential side effects. These side effects can range from drowsiness and dizziness to gastrointestinal disturbances and weight gain. Therefore, it is crucial for healthcare professionals to carefully monitor the use of these medications and adjust the dosage as needed.
Physical Therapy Techniques
In addition to medications, physical therapy techniques can provide temporary pain relief for individuals with mandibular nerve pain. Heat or cold therapy, for example, can help relax the muscles and reduce inflammation in the affected area. Applying a warm compress or an ice pack to the jaw can help alleviate pain and promote healing.
Another physical therapy technique that can be beneficial is ultrasound therapy. This involves the use of sound waves to generate heat deep within the tissues, which can help reduce pain and inflammation. Additionally, transcutaneous electrical nerve stimulation (TENS) is a technique that involves the use of low-voltage electrical currents to stimulate the nerves and provide pain relief.
These physical therapy techniques not only help alleviate pain but also stimulate the release of endorphins, which are the body’s natural pain-relieving substances. This can provide individuals with a sense of well-being and improve their overall quality of life.
Alternative Therapies
Complementary and alternative therapies have gained popularity in recent years as potential treatments for mandibular nerve pain. These therapies include acupuncture, mindfulness-based stress reduction, and the use of herbal remedies.
Acupuncture, an ancient Chinese practice, involves the insertion of thin needles into specific points on the body. This is believed to stimulate the flow of energy and promote healing. Some individuals with mandibular nerve pain have reported positive results with acupuncture, experiencing a reduction in pain and improved jaw function.
Mindfulness-based stress reduction techniques, such as meditation and deep breathing exercises, can also be helpful in managing mandibular nerve pain. By focusing on the present moment and cultivating a sense of calm, individuals can reduce stress and tension, which can contribute to pain relief.
Herbal remedies, such as chamomile and lavender, have also been explored for their potential benefits in managing mandibular nerve pain. These herbs have natural anti-inflammatory and analgesic properties, which can help reduce pain and promote relaxation.
While some individuals may find these alternative therapies beneficial, it is important to consult with a healthcare professional before integrating them into the treatment plan. This ensures that the therapies are safe and appropriate for the individual’s specific condition.
In conclusion, non-surgical treatment options for mandibular nerve pain encompass a range of approaches, including medications, physical therapy techniques, and alternative therapies. These options provide individuals with choices in managing their pain and improving their quality of life. It is important for healthcare professionals to work closely with patients to develop a personalized treatment plan that addresses their unique needs and preferences.
Surgical Treatments for Mandibular Nerve Pain
In cases where non-surgical treatment options fail to provide adequate pain relief or if there is an identifiable structural abnormality causing the pain, surgical interventions may be considered.
When is Surgery Necessary?
Surgery may be necessary when:
- Non-surgical treatments have been ineffective
- There is evidence of a compressive lesion on imaging studies
- The individual’s quality of life is significantly impaired
It is crucial to have a detailed discussion with a healthcare professional to weigh the benefits and potential risks of surgical interventions.
Types of Surgery for Mandibular Nerve Pain
There are several surgical procedures that can be considered for the management of mandibular nerve pain, including:
- Microvascular decompression: Involves placing a cushioning material between the nerve and the compressing blood vessel.
- Radiofrequency ablation: Uses heat or cold to disrupt the pain signals along the nerve fibers.
- Glycerol injection: A small amount of glycerol is injected into the trigeminal ganglion to prevent pain signals from being transmitted.
Each surgical option has its own benefits, risks, and potential outcomes. A healthcare professional will help determine the most appropriate surgical approach based on individual circumstances.
Living with Mandibular Nerve Pain
Managing mandibular nerve pain requires a multimodal approach that extends beyond medical interventions. Making certain lifestyle modifications and establishing effective coping mechanisms can positively impact an individual’s overall well-being.
Lifestyle Modifications
Adopting healthy habits, such as practicing good oral hygiene, avoiding excessive caffeine consumption, and maintaining a balanced diet, can help minimize triggers and reduce the likelihood of pain episodes. Additionally, incorporating stress-reducing techniques, such as meditation and gentle exercise, may promote overall relaxation and pain management.
Coping Mechanisms and Support Systems
Living with chronic pain can be challenging, both physically and emotionally. Finding effective coping mechanisms, such as maintaining a positive outlook, engaging in activities that bring joy, and seeking support from loved ones or support groups, can help individuals navigate the complex emotional landscape associated with mandibular nerve pain.
Prevention of Mandibular Nerve Pain
While mandibular nerve pain cannot always be prevented, certain measures can reduce the risk of developing or worsening the condition.
Regular Dental Check-ups
Regular visits to a dentist for routine check-ups and proper oral hygiene can help identify and address any dental conditions that may contribute to mandibular nerve pain. Early identification and treatment of dental issues can significantly reduce the risk of developing or exacerbating symptoms.
Healthy Lifestyle Choices
Maintaining a healthy lifestyle, including practicing stress management techniques, getting adequate sleep, and avoiding excessive alcohol and tobacco use, can promote overall well-being and potentially lessen the risk of mandibular nerve pain.
Conclusion: Managing Mandibular Nerve Pain
Mandibular nerve pain, or trigeminal neuralgia, can significantly impact an individual’s quality of life. Understanding the anatomy, symptoms, and treatment options associated with this condition is crucial for effective management. It is important to consult with a healthcare professional for proper diagnosis, personalized treatment plans, and ongoing support. Through a collaborative approach between healthcare providers and individuals living with mandibular nerve pain, it is possible to navigate the challenges of this condition and improve overall well-being.