how to give mandibular nerve block
The mandibular nerve block is a commonly performed procedure in dentistry. By effectively numbing the mandibular nerve, dentists can ensure their patients remain comfortable during various dental treatments. This article will serve as a step-by-step guide on how to give a mandibular nerve block, exploring the anatomy and function of the mandibular nerve, necessary preparations, the injection procedure itself, post-procedure care, safety measures, and frequently asked questions.
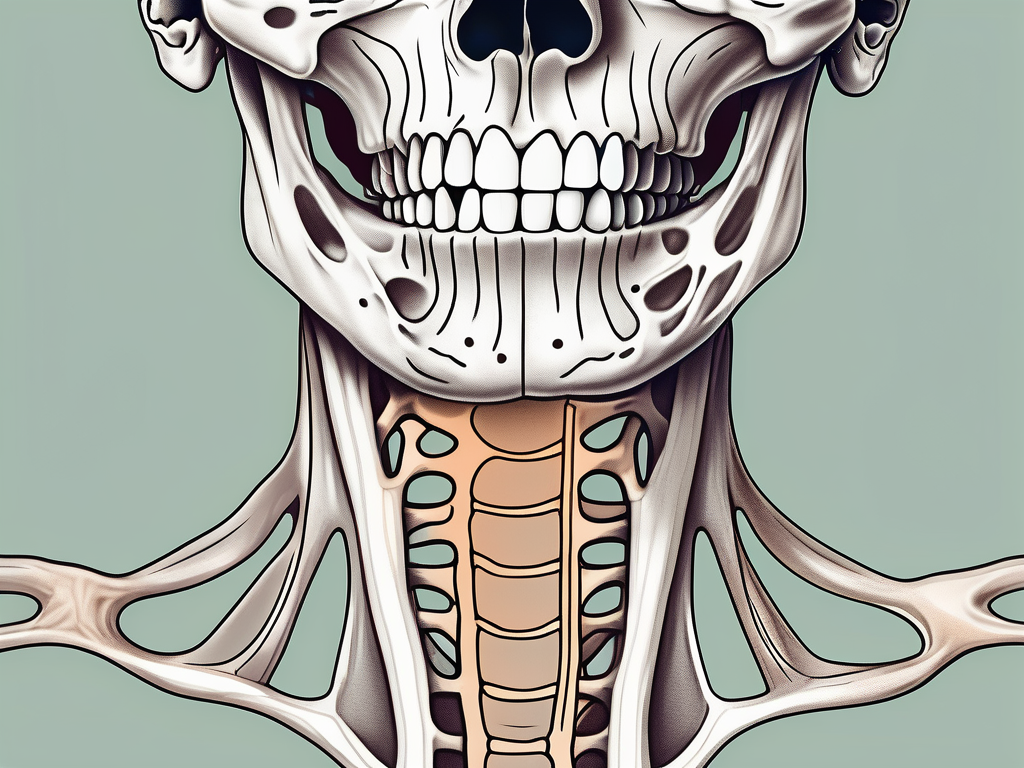
Understanding the Mandibular Nerve
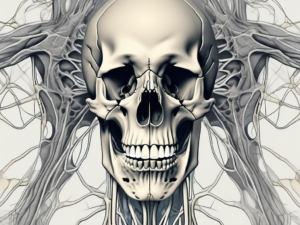
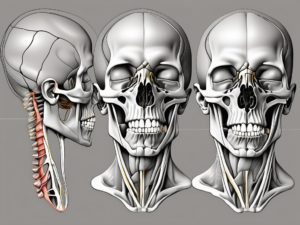
The mandibular nerve, a branch of the trigeminal nerve, plays a crucial role in dental anesthesia. It supplies sensory innervation to the lower lip, chin, lower teeth, gingiva, and the anterior two-thirds of the tongue. Understanding the anatomy and function of the mandibular nerve is essential for safe and effective administration of a mandibular nerve block.
The mandibular nerve, also known as the V3 branch of the trigeminal nerve, is the largest of the three divisions. It originates from the trigeminal ganglion, located in the middle cranial fossa, and exits the skull through the foramen ovale. Once outside the skull, the mandibular nerve enters the infratemporal fossa, where it gives rise to several important branches.
Anatomy of the Mandibular Nerve
The mandibular nerve traverses through the foramina in the skull and enters the infratemporal fossa. It then branches into several divisions, including the buccal, lingual, and inferior alveolar nerves. Familiarizing yourself with the course of the mandibular nerve and its innervation areas is fundamental to the success of a mandibular nerve block.
The buccal nerve, one of the branches of the mandibular nerve, provides sensory innervation to the buccal mucosa, the skin of the cheek, and the buccal gingiva. It also supplies motor fibers to the buccinator muscle, which plays a crucial role in mastication and facial expression.
The lingual nerve, another branch of the mandibular nerve, carries sensory information from the anterior two-thirds of the tongue, as well as the floor of the mouth and the lingual gingiva. It also provides taste sensation to the same areas, except for the circumvallate papillae, which are innervated by the glossopharyngeal nerve.
The inferior alveolar nerve, the largest branch of the mandibular nerve, supplies sensory innervation to the lower teeth, gingiva, and the lower lip. It also provides motor fibers to the muscles of mastication, including the masseter, temporalis, and medial pterygoid muscles.
Function of the Mandibular Nerve
The mandibular nerve carries both sensory and motor fibers. While our focus is on blocking the sensory innervation, it is crucial to be mindful of the motor function to avoid potential complications. The motor fibers of the mandibular nerve innervate the muscles of mastication and other facial muscles.
The muscles of mastication, including the masseter, temporalis, and medial pterygoid muscles, are responsible for the movement of the mandible during chewing and biting. The motor fibers of the mandibular nerve ensure the proper functioning of these muscles, allowing for efficient mastication and proper alignment of the teeth.
In addition to the muscles of mastication, the mandibular nerve also supplies motor fibers to other facial muscles, including the tensor tympani muscle, which is responsible for dampening loud sounds, and the tensor veli palatini muscle, which plays a role in opening the auditory tube during swallowing and yawning.
Understanding the function of the mandibular nerve and its motor innervation is important when administering a mandibular nerve block to ensure that the motor function is not compromised. Careful technique and accurate placement of the anesthetic solution can help avoid potential complications and ensure successful anesthesia of the sensory fibers.
Preparing for the Procedure
Proper preparation is key to ensuring a smooth and safe mandibular nerve block procedure. This section will outline the necessary equipment and materials, as well as the steps required to prepare the patient for the injection.
Administering a mandibular nerve block requires careful attention to detail and a thorough understanding of the procedure. By following the proper preparation steps, dental professionals can ensure the comfort and safety of their patients.
Necessary Equipment and Materials
Before administering a mandibular nerve block, gather all the necessary equipment and materials. This includes sterile gloves, local anesthetic (such as lidocaine with epinephrine), a syringe, a needle appropriate for the technique, gauze, and a sharps container. Ensuring that all equipment is in pristine condition and sterile is essential for patient safety.
Sterile gloves are crucial to prevent any contamination during the procedure. Local anesthetic, such as lidocaine with epinephrine, is commonly used to numb the injection site and minimize discomfort for the patient. The syringe and needle must be appropriate for the technique being used, ensuring accurate delivery of the anesthetic. Gauze is necessary to control any bleeding that may occur, and a sharps container is essential for the safe disposal of used needles.
Patient Preparation and Positioning
Prior to any dental procedure, including a mandibular nerve block, proper patient preparation is vital. Explain the procedure to the patient, addressing any concerns or questions they may have. Building trust and ensuring open communication can help alleviate anxiety and create a more comfortable environment.
Once the patient is informed about the procedure, it is important to position them in a way that maximizes their comfort and allows for easy access to the injection site. The dental chair should be reclined to a suitable angle, providing both support and relaxation for the patient. Adequate lighting is crucial for the dental professional to visualize the injection site accurately. Ensuring visibility of the injection site is essential for a successful mandibular nerve block.
Additionally, it is important to consider the patient’s overall well-being during the procedure. Providing a calm and soothing environment can help reduce stress and promote a positive experience. Taking the time to address any specific patient needs or preferences can further enhance their comfort and overall satisfaction.
Step-by-Step Guide to Administering a Mandibular Nerve Block
Administering a mandibular nerve block requires precision and careful technique. This section will guide you through the step-by-step process, from locating the injection site to performing the injection.
Locating the Injection Site
Proper identification of the injection site is crucial for the success and safety of a mandibular nerve block. The most common technique involves targeting the pterygomandibular raphe. This bilateral fibrous band marks the insertion point of the buccinator muscle onto the posterior mandible. Palpate the area and locate the raphe, ensuring your orientation and anatomical landmarks are accurate.
The pterygomandibular raphe is an important landmark because it serves as a reliable guide for locating the inferior alveolar nerve, which is the target for the mandibular nerve block. This nerve provides sensory innervation to the lower teeth, lower lip, and chin. By accurately identifying the raphe, you can ensure that the injection will be delivered in close proximity to the nerve, maximizing the effectiveness of the block.
When palpating the area, pay attention to the patient’s comfort level and any signs of tenderness or inflammation. This information can help you determine if there are any contraindications or complications that may affect the administration of the nerve block.
Performing the Injection
Once the injection site has been identified, clean the area with an antiseptic solution, further ensuring patient safety and minimizing the risk of complications. It is important to maintain a sterile environment to prevent the introduction of bacteria or other contaminants into the injection site.
Before inserting the needle, it is essential to choose the appropriate size and gauge for the injection. The needle should be long enough to reach the target area but not so long that it poses a risk of injury to surrounding structures. The gauge of the needle should be selected based on the viscosity of the anesthetic solution and the desired rate of injection.
Using a steady hand, insert the needle into the tissue, maintaining a necessary depth and direction. Take care to avoid any major blood vessels or nerves in the area. Aspirate to ensure proper needle placement, checking for any signs of blood return. If blood is aspirated, reposition the needle to avoid intravascular injection.
Once proper needle placement is confirmed, administer the anesthetic slowly and steadily. This allows for a gradual diffusion of the anesthetic solution, reducing the risk of complications such as nerve damage or excessive spread of the anesthetic. Keep patient comfort in mind throughout the procedure, adjusting your approach as needed. Communicate with the patient and monitor their responses to ensure their well-being and comfort.
After the injection, observe the patient for any signs of adverse reactions or complications. These may include numbness, tingling, or difficulty speaking or swallowing. Provide appropriate post-injection instructions to the patient, including any necessary precautions or follow-up care.
Remember, administering a mandibular nerve block requires a thorough understanding of the anatomy and technique involved. Practice proper sterile technique and maintain clear communication with the patient throughout the procedure. By following these steps and guidelines, you can ensure the safe and effective administration of a mandibular nerve block.
Post-Procedure Care
After successfully administering the mandibular nerve block, appropriate post-procedure care is essential. This section will address how to monitor the patient and manage any potential complications that may arise.
It is important to note that the mandibular nerve block is a commonly performed procedure in dentistry, used to provide anesthesia to the lower jaw and teeth. This type of anesthesia is typically administered for various dental procedures, such as tooth extractions, root canals, and dental implant placements.
Following the injection, closely monitor the patient for any adverse reactions or complications. Keep a record of vital signs, including blood pressure, heart rate, and oxygen saturation levels. Additionally, evaluate the patient’s level of anesthesia, ensuring that they are comfortable and pain-free throughout the procedure.
Proper monitoring will allow for timely identification and management of any challenges that may arise. It is crucial to have a trained dental professional or an anesthesiologist present during the procedure to ensure patient safety and to address any complications promptly.
Monitoring the Patient
Monitoring the patient after a mandibular nerve block is crucial for their well-being. While the procedure itself is generally safe, there are potential risks and complications that need to be monitored and managed effectively.
One potential complication that may occur is hematoma formation. A hematoma is a localized collection of blood outside the blood vessels, usually caused by bleeding during the injection. It is important to assess the injection site for any signs of swelling, discoloration, or pain, as these may indicate the presence of a hematoma. If a hematoma is suspected, appropriate measures should be taken to manage it, such as applying ice packs to reduce swelling and providing pain relief medications if necessary.
Another potential complication is accidental intravascular injection, where the anesthetic solution is inadvertently injected into a blood vessel. This can lead to systemic effects, such as cardiovascular and central nervous system complications. It is crucial to monitor the patient for any signs of systemic toxicity, including dizziness, confusion, rapid heart rate, or changes in blood pressure. If these symptoms occur, immediate intervention is necessary, and the patient should be closely monitored until the effects subside.
Managing potential complications requires a comprehensive understanding of the anatomy and physiology of the mandibular region. Dental professionals should be well-versed in the techniques and protocols necessary to handle any complications that may arise during or after the procedure.
Managing Potential Complications
While mandibular nerve blocks are generally safe, complications can occasionally occur. Familiarize yourself with potential complications, such as hematoma formation or accidental intravascular injection, and be prepared to manage them accordingly.
In addition to hematoma formation and accidental intravascular injection, other potential complications include infection at the injection site, nerve damage, or allergic reactions to the anesthetic agent. These complications, though rare, should be considered and managed appropriately.
If an infection occurs at the injection site, it is important to promptly administer appropriate antibiotics and provide proper wound care. Nerve damage, although rare, can lead to temporary or permanent sensory or motor deficits. If nerve damage is suspected, a referral to a specialist may be necessary for further evaluation and management.
Allergic reactions to the anesthetic agent used in the mandibular nerve block can range from mild to severe. It is essential to have emergency medications and equipment readily available to manage any allergic reactions effectively. This may include antihistamines, corticosteroids, and in severe cases, epinephrine to counteract anaphylaxis.
Should any complications arise, it is crucial to act quickly and consult with an experienced dental professional to ensure the best course of action. Prompt intervention and appropriate management can help minimize the impact of complications and promote optimal patient outcomes.
Safety Measures and Best Practices
Maintaining a high level of safety during the administration of a mandibular nerve block is of utmost importance. This section will discuss essential safety measures and best practices that should be followed consistently.
When it comes to safety, there are several key factors that need to be considered. One of the most critical aspects is sterilization and hygiene. Proper sterilization of equipment and maintaining strict hygiene practices is crucial to prevent infection and ensure patient safety. This includes not only the sterilization of equipment but also the use of gloves, needles, and syringes. Following recommended protocols for sterilization is essential to minimize the risk of contamination and maintain a sterile environment.
Another important aspect of safety during a mandibular nerve block is patient comfort and communication. Establishing open and effective communication with the patient is essential in providing a comfortable experience. It is important to prioritize patient comfort throughout the procedure by addressing their concerns, answering their questions, and ensuring they are informed about the process. This can help alleviate anxiety and build trust between the patient and the healthcare provider.
During the procedure, it is important to continuously monitor the patient’s comfort level and encourage them to communicate any discomfort or signs of adverse reactions. This can include asking the patient if they are experiencing any pain or discomfort, and ensuring that they are aware of the steps that can be taken to alleviate any discomfort they may be feeling.
Additionally, it is crucial to have a thorough understanding of the anatomy and physiology of the mandibular nerve. This knowledge will help ensure accurate placement of the nerve block and reduce the risk of complications. Healthcare providers should stay up to date with the latest research and guidelines regarding mandibular nerve blocks to ensure they are following the best practices.
Lastly, it is important to have a comprehensive emergency plan in place in case any complications arise during the procedure. This includes having the necessary equipment and medications readily available to manage any potential adverse reactions or emergencies.
In conclusion, maintaining safety during the administration of a mandibular nerve block requires adherence to strict sterilization and hygiene practices, effective communication with the patient, continuous monitoring of their comfort level, and a thorough understanding of the anatomy and physiology involved. By following these best practices, healthcare providers can ensure the safety and well-being of their patients.
Frequently Asked Questions about Mandibular Nerve Blocks
To provide a comprehensive understanding of mandibular nerve blocks, this section will address frequently asked questions regarding their necessity, risks, and side effects.
When is a Mandibular Nerve Block Necessary?
Mandibular nerve blocks are commonly used in dental procedures to ensure patient comfort. They are particularly necessary for extensive dental work, such as extractions, restorative treatments, and oral surgery, where substantial anesthesia is required to numb the lower teeth, gingiva, lip, and tongue.
What are the Risks and Side Effects?
As with any medical procedure, mandibular nerve blocks carry potential risks and side effects. These can include temporary numbness, bruising, swelling, or more severe complications such as hematoma formation or nerve damage. It is crucial to educate patients about these possibilities and consult with an experienced dental professional to address any concerns.
Administering a mandibular nerve block is a valuable skill for any dental professional. By following proper procedures, ensuring patient comfort, and prioritizing safety, dentists can carry out this procedure effectively. Nonetheless, always consult with an experienced dental professional or oral surgeon before performing any invasive procedure. Together, let us strive for delivering optimal patient care in every dental setting.