how to prevent mandibular nerve injury
Mandibular nerve injury is a serious concern that can have significant impacts on a person’s overall well-being. Understanding the anatomy, functions, and common causes of mandibular nerve injury is crucial in preventing such injuries. By implementing effective prevention strategies and staying informed about the latest research and developments, individuals can take proactive measures to minimize the risk of mandibular nerve injury.
Understanding the Mandibular Nerve
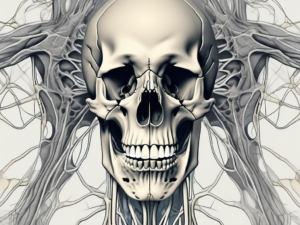
The mandibular nerve is a fascinating and vital component of the trigeminal nerve, which is responsible for providing sensory innervation to the face. Specifically, the mandibular nerve is the largest branch of the trigeminal nerve and plays a crucial role in the functioning of the lower jaw, lower teeth, and gums.
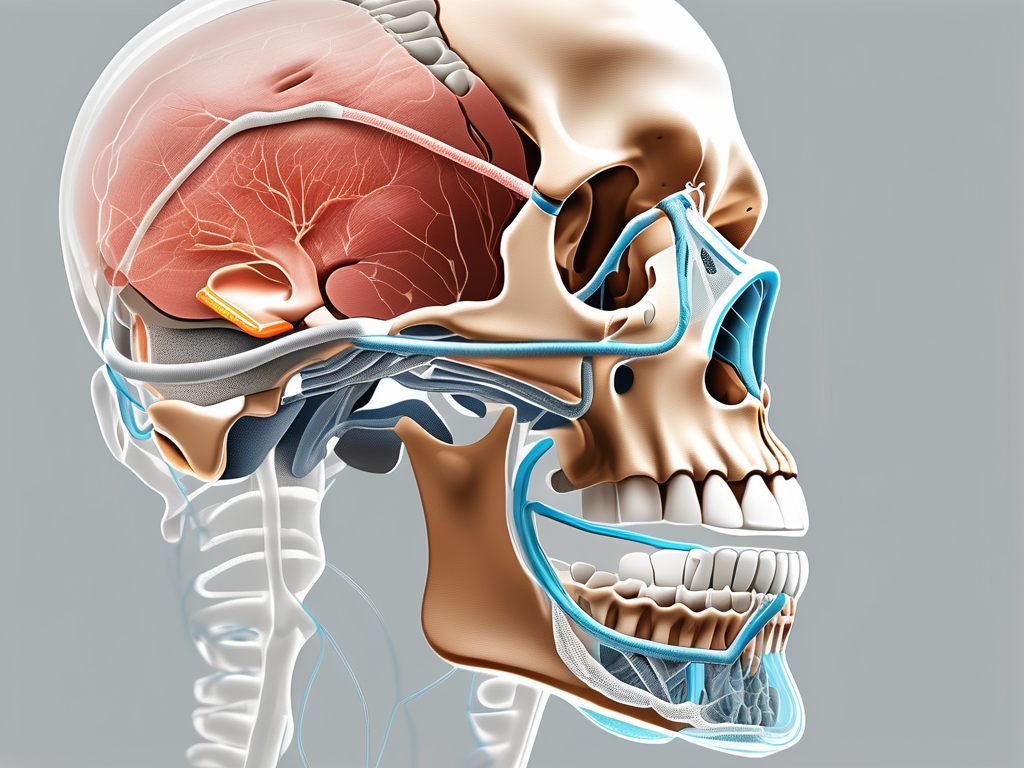
Anatomy of the Mandibular Nerve
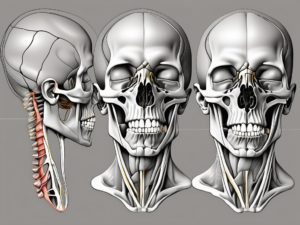
To truly appreciate the complexity and significance of the mandibular nerve, it is important to understand its intricate anatomy. This remarkable nerve passes through the mandibular notch in the skull, traversing a path that allows it to supply sensory and motor fibers to various regions of the face.
As the mandibular nerve courses through the skull, it branches out into multiple smaller nerves, each with its own specific function. These branches include the inferior alveolar nerve, which provides sensory innervation to the lower teeth and gums, and the lingual nerve, which supplies sensation to the anterior two-thirds of the tongue.
In addition to its sensory role, the mandibular nerve also plays a crucial role in motor function. It supplies motor fibers to the muscles responsible for chewing, known as the muscles of mastication. These muscles, including the masseter, temporalis, and medial and lateral pterygoids, work in harmony to facilitate the process of chewing and maintain jaw movement.
Functions of the Mandibular Nerve
The mandibular nerve is a sensory powerhouse, allowing individuals to perceive touch, pain, temperature, and proprioception in the lower face. Without the mandibular nerve, simple tasks such as biting into an apple or feeling the warmth of a hot beverage would be impossible.
Furthermore, the mandibular nerve’s role in motor function is equally significant. The muscles of mastication, innervated by the mandibular nerve, are responsible for the mechanical breakdown of food during the process of chewing. This crucial step in digestion ensures that food particles are adequately prepared for further digestion and absorption in the gastrointestinal tract.
Moreover, the mandibular nerve enables the intricate movements of the jaw, allowing for actions such as grinding, clenching, and lateral movements. These movements are essential for proper mastication and contribute to the overall efficiency of the digestive process.
In summary, the mandibular nerve is a remarkable component of the trigeminal nerve, with its intricate anatomy and multifaceted functions. From providing sensory innervation to the lower face to facilitating the process of chewing, this nerve plays an indispensable role in our everyday lives. The complexity and significance of the mandibular nerve highlight the remarkable intricacies of the human body and the wonders of neuroscience.
Common Causes of Mandibular Nerve Injury
Dental Procedures and Risks
Dental procedures, such as extractions, root canal treatments, and dental implant surgery, carry potential risks of mandibular nerve injury. This can occur due to accidental damage to the nerve during the procedure, particularly if the dentist is inexperienced or fails to exercise proper care. It is essential to choose a qualified and experienced dentist and discuss the potential risks and benefits of any dental procedure before proceeding.
In addition to accidental damage, there are other factors that can increase the risk of mandibular nerve injury during dental procedures. For example, the position of the nerve in relation to the tooth being treated can vary from person to person. If the nerve is located close to the tooth or in an abnormal position, there is a higher chance of injury. Furthermore, certain medical conditions, such as a history of nerve disorders or previous nerve injuries, can make the nerve more susceptible to damage.
Moreover, the use of improper dental instruments or techniques can also contribute to mandibular nerve injury. Dentists must ensure that they are using the correct tools and employing appropriate techniques to minimize the risk of nerve damage. This highlights the importance of continuous education and training for dental professionals to stay updated with the latest advancements in dental procedures and techniques.
Trauma and Accidents
Trauma or accidents involving the face and jaw can lead to mandibular nerve injury. High-impact injuries, such as motor vehicle accidents or sports-related trauma, can cause damage to the nerves. It is important to take necessary precautions to prevent accidents, such as wearing appropriate protective gear when engaging in activities with a risk of facial injury.
Furthermore, the severity of the trauma can play a role in the likelihood of mandibular nerve injury. For instance, a direct blow to the jaw may result in nerve damage if the force is significant enough to cause fractures or dislocations. In some cases, the nerve may be compressed or stretched during the trauma, leading to temporary or permanent impairment.
It is worth noting that the mandibular nerve is not the only nerve at risk during facial trauma. The facial nerve, which controls facial expressions, and other sensory nerves in the face can also be affected. Therefore, prompt medical attention is crucial in cases of facial trauma to assess and address any potential nerve injuries.
Additionally, certain individuals may be more prone to mandibular nerve injury due to anatomical variations. For example, people with a smaller jaw or a more prominent mandibular angle may have less protection for the nerve, making them more susceptible to injury during accidents or trauma.
Symptoms of Mandibular Nerve Injury
Physical Symptoms
Mandibular nerve injuries can manifest through various physical symptoms, including numbness or tingling in the lower lip, chin, or gums. Some individuals may experience pain or a burning sensation in these areas. Additionally, there may be difficulties with jaw movement, leading to problems with chewing and speech.
When the mandibular nerve is injured, it can disrupt the normal functioning of the muscles and tissues in the lower part of the face. This can result in a loss of sensation or altered sensation in the affected areas. Numbness or tingling sensations may be constant or intermittent, and they can range from mild to severe.
In some cases, individuals with mandibular nerve injuries may also experience pain or a burning sensation in the lower lip, chin, or gums. This discomfort can be persistent or occur in episodes, making it difficult for individuals to carry out their daily activities comfortably.
Furthermore, difficulties with jaw movement are common in mandibular nerve injuries. The affected individuals may find it challenging to open or close their mouths fully, leading to problems with chewing and speech. This can have a significant impact on their ability to eat, communicate, and engage in social interactions.
Emotional and Psychological Impact
Mandibular nerve injury can have a profound emotional and psychological impact on individuals. Chronic pain, functional limitations, and changes in facial sensation can result in anxiety, depression, or decreased quality of life. Seeking support from mental health professionals or support groups can be invaluable in coping with these challenges.
The emotional and psychological impact of mandibular nerve injury should not be underestimated. Chronic pain, which is often associated with this type of injury, can lead to feelings of frustration, helplessness, and even despair. The constant discomfort and limitations in daily activities can significantly affect an individual’s overall well-being and quality of life.
Moreover, the functional limitations caused by mandibular nerve injury can also contribute to emotional distress. Difficulties with chewing and speech can make it challenging for individuals to eat their favorite foods or communicate effectively with others. These limitations can lead to feelings of isolation, frustration, and a loss of confidence in social situations.
Changes in facial sensation can further exacerbate the emotional and psychological impact of mandibular nerve injury. The altered sensation in the lower lip, chin, or gums can be unsettling and may affect an individual’s self-image and self-esteem. This can result in feelings of self-consciousness and a negative body image.
It is important for individuals with mandibular nerve injuries to seek support from mental health professionals or support groups. These resources can provide a safe space to express emotions, learn coping strategies, and connect with others who are going through similar experiences. Building a strong support network can help individuals navigate the emotional and psychological challenges associated with mandibular nerve injury.
Prevention Strategies for Mandibular Nerve Injury
Precautions during Dental Procedures
When undergoing dental procedures, it is essential to ensure that the dental professional takes appropriate precautions to minimize the risk of mandibular nerve injury. This includes conducting a thorough assessment of the patient’s anatomy, using imaging techniques when necessary, and employing proper surgical techniques. Dentists are trained to carefully examine the patient’s oral cavity and surrounding structures to identify any potential risks or abnormalities that may increase the likelihood of nerve injury. By utilizing advanced imaging technologies, such as cone beam computed tomography (CBCT), dentists can obtain detailed three-dimensional images of the patient’s jaw and nerve pathways, allowing for precise planning and execution of dental procedures.
In addition to the assessment and imaging techniques, dentists also employ various surgical techniques to minimize the risk of mandibular nerve injury. For instance, during procedures involving the extraction of impacted wisdom teeth, dentists may opt for a surgical approach that involves sectioning the tooth and removing it in smaller fragments. This technique reduces the amount of force required for extraction, thereby minimizing the risk of nerve injury. Dentists also utilize specialized instruments and tools designed to facilitate precise and controlled movements during surgical procedures, further reducing the chances of nerve damage.
Furthermore, open communication between the patient and the dentist is crucial in preventing mandibular nerve injury. Patients should feel comfortable discussing any concerns or fears they may have regarding the procedure. By openly communicating their worries, patients can gain a better understanding of the potential risks involved and the steps taken by the dentist to mitigate those risks. Dentists, on the other hand, should be attentive and receptive to their patients’ concerns, providing clear explanations and reassurance throughout the treatment process.
Safety Measures to Avoid Accidents
Preventing accidents that may lead to mandibular nerve injury requires being mindful of safety measures. While dental procedures are performed under controlled conditions, accidents can occur in various other situations. For instance, engaging in sports or recreational activities that carry a risk of facial trauma, such as contact sports or extreme sports, necessitates the use of protective gear. Wearing helmets, face masks, or mouthguards can significantly reduce the chances of sustaining facial injuries, including mandibular nerve damage.
Moreover, taking precautions in everyday life can also help minimize the risk of accidental falls and injuries that may affect the mandibular nerve. Maintaining well-lit walkways and staircases at home can prevent trips and falls, reducing the likelihood of facial trauma. Promptly addressing any potential hazards, such as loose rugs or uneven surfaces, can also contribute to a safer environment. Additionally, practicing good oral hygiene and visiting the dentist regularly for check-ups and cleanings can help prevent dental issues that may require invasive procedures, thus reducing the risk of mandibular nerve injury.
In conclusion, preventing mandibular nerve injury involves a combination of precautions taken during dental procedures and safety measures in everyday life. Dental professionals play a crucial role in minimizing the risk of nerve damage through thorough assessments, advanced imaging techniques, and precise surgical approaches. Patients, on the other hand, should actively engage in open communication with their dentists and adhere to safety measures, such as wearing protective gear and maintaining a safe environment, to prevent accidents that may lead to mandibular nerve injury.
Treatment Options for Mandibular Nerve Injury
A mandibular nerve injury can be a distressing condition that affects the functionality and sensation of the lower jaw. It can result from various causes, including trauma, dental procedures, or underlying medical conditions. Fortunately, there are several treatment options available to address this condition and alleviate the associated symptoms.
Non-Surgical Treatments
In mild cases of mandibular nerve injury, the condition may improve without the need for surgical intervention. Non-surgical treatments can be effective in managing the symptoms and promoting the natural healing process.
Pain management techniques play a crucial role in providing relief to individuals suffering from mandibular nerve injuries. These techniques may include the use of heat or cold therapy, transcutaneous electrical nerve stimulation (TENS), or acupuncture. By targeting the affected area, these methods can help reduce pain and discomfort.
Physical therapy is another non-surgical treatment option that can aid in the recovery of mandibular nerve injuries. Through specific exercises and stretches, physical therapists can help improve jaw mobility, strengthen surrounding muscles, and enhance overall jaw function. This approach is particularly beneficial for individuals experiencing limited jaw movement or difficulty in performing daily activities such as eating or speaking.
Additionally, medications may be prescribed to manage the symptoms associated with mandibular nerve injuries. Anti-inflammatory drugs can help reduce inflammation around the affected nerve, alleviating pain and swelling. In cases where neuropathic pain is present, medications such as anticonvulsants or antidepressants may be recommended to target the underlying nerve-related pain signals.
It is important to note that the appropriate treatment option for a mandibular nerve injury can vary depending on the individual case. Therefore, it is crucial to consult with a healthcare professional who specializes in this area for a proper diagnosis and personalized treatment plan.
Surgical Interventions
In more severe cases of mandibular nerve injury, non-surgical treatments may not be sufficient to restore normal nerve function. Surgical interventions may then be necessary to repair the damaged nerves or relieve any compression on the nerve.
When considering surgical options, it is essential to seek the expertise of experienced surgeons who specialize in oral and maxillofacial surgery. These professionals possess the knowledge and skills required to perform intricate procedures with precision and care.
Surgical procedures for mandibular nerve injuries can involve nerve repair or decompression. Nerve repair aims to reconnect or reconstruct damaged nerve fibers, allowing for the restoration of nerve function. This procedure requires meticulous planning and delicate surgical techniques to ensure optimal outcomes.
In cases where compression on the mandibular nerve is the primary cause of injury, decompression surgery may be performed. This procedure involves relieving the pressure on the nerve by removing any surrounding structures or tissues that may be compressing it. By eliminating the compression, the nerve can regain its normal function and alleviate associated symptoms.
It is important to note that surgical interventions for mandibular nerve injuries carry their own risks and potential complications. Therefore, thorough evaluation and discussion with the healthcare professional are crucial to determine the most appropriate course of action.
In conclusion, treatment options for mandibular nerve injuries can range from non-surgical approaches to surgical interventions. The choice of treatment depends on the severity of the injury and the individual’s specific circumstances. Consulting with a healthcare professional who specializes in this area is essential to receive an accurate diagnosis and develop a personalized treatment plan that addresses the unique needs of each patient.
Recovery and Rehabilitation from Mandibular Nerve Injury
Physical Therapy and Exercises
Following a mandibular nerve injury, a comprehensive rehabilitation plan may involve physical therapy to improve jaw movement, strengthen muscles, and restore function. Physiotherapists can guide individuals through exercises tailored to their specific condition, helping to regain optimal oral function and minimize long-term complications.
Coping Mechanisms and Support Systems
Coping with the challenges posed by a mandibular nerve injury is easier when individuals have access to adequate support systems. Engaging in supportive activities, such as joining support groups or seeking counseling, can provide emotional support and help individuals navigate the physical and emotional impact of the injury.
Future Research and Developments in Mandibular Nerve Injury Prevention
Technological Advancements
Ongoing research and technological advancements hold promising prospects for the prevention and management of mandibular nerve injury. Improved imaging techniques, such as 3D imaging and virtual reality simulations, can aid in assessing anatomical variations and planning procedures with enhanced precision. Additionally, developments in surgical techniques and materials may further reduce the risks associated with mandibular nerve injury.
Ongoing Clinical Trials and Research
Continued research efforts, including clinical trials, are crucial in advancing our understanding of mandibular nerve injury prevention and treatment. Participating in clinical trials, when appropriate, can contribute to the progress of medical science and potentially provide individuals with access to innovative treatments. It is important to stay informed about ongoing research and consult with healthcare professionals to explore suitable options.
Conclusion
Preventing mandibular nerve injury requires a comprehensive approach that combines education, awareness, and proactive measures. By understanding the anatomy and functions of the mandibular nerve, being aware of the common causes and symptoms of mandibular nerve injury, implementing effective prevention strategies, and staying informed about the latest research and developments, individuals can empower themselves and reduce the risk of mandibular nerve injury. If you have concerns or experience any symptoms related to mandibular nerve injury, it is crucial to consult with a healthcare professional for proper diagnosis and guidance.