how to prevent mandibular nerve injury during surgery
Mandibular nerve injury is a potential complication that surgeons and patients alike hope to avoid during surgical procedures. The mandibular nerve, also known as the inferior alveolar nerve, plays a vital role in the innervation of the lower face and mandibular teeth. Damage to this nerve can result in severe sensory disturbances, including numbness and pain, as well as functional impairments. However, with proper understanding, preoperative planning, and surgical techniques, the risk of mandibular nerve injury can be minimized.
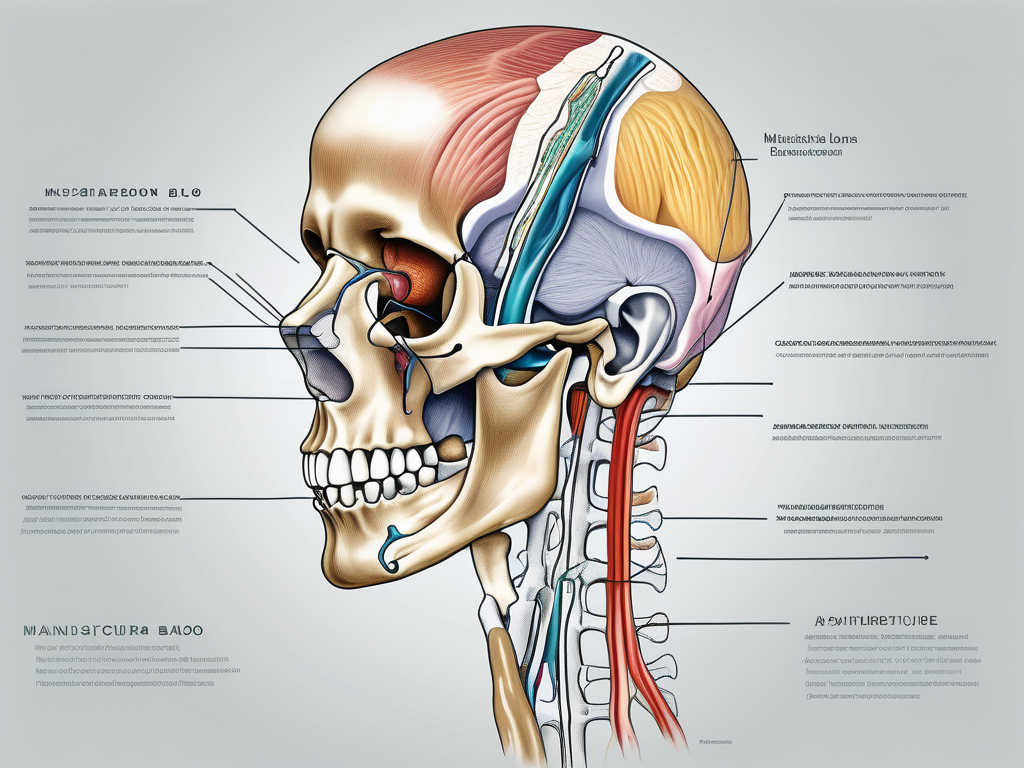
Understanding the Mandibular Nerve Structure
Anatomy of the Mandibular Nerve
Before delving into the prevention of mandibular nerve injury, it is essential to have a thorough understanding of its anatomy. The mandibular nerve is the largest branch of the trigeminal nerve, a key sensory nerve in the head and neck region. Originating from the trigeminal ganglion, it descends through the skull, passes through the mandibular foramen, and splits into various branches that innervate the lower face, mandibular teeth, and temporomandibular joint.
The course of the mandibular nerve is complex, as it passes through various bony structures and closely interacts with important anatomical landmarks. The proximity of the nerve to structures such as the mandibular canal and the lingual nerve increases the risk of injury during surgical procedures. Therefore, a thorough familiarity with the nerve’s anatomical relationships is crucial for surgical success.
As the mandibular nerve descends through the skull, it traverses the petrous part of the temporal bone, which houses the middle and inner ear structures. This close proximity to the auditory system highlights the importance of precision and caution during surgical interventions near the mandibular nerve.
Upon passing through the mandibular foramen, the mandibular nerve enters the mandibular canal, a bony tunnel within the mandible. This canal not only provides protection to the nerve but also serves as a conduit for blood vessels that supply the lower teeth and surrounding tissues. The intricate relationship between the mandibular nerve and the mandibular canal necessitates meticulous surgical planning to avoid any inadvertent damage.
Once inside the mandibular canal, the mandibular nerve gives rise to several branches that innervate different regions of the lower face. These branches include the buccal nerve, which supplies sensation to the cheek, the mental nerve, responsible for innervating the chin and lower lip, and the inferior alveolar nerve, which provides sensory input to the mandibular teeth and gums.
Importance of the Mandibular Nerve in Facial Functions
The mandibular nerve is vital for sensory and motor functions in the lower face. It provides innervation to the lip, chin, gingiva, and teeth, allowing for the perception of touch, temperature, and pain. Moreover, the mandibular nerve controls the movements of the muscles responsible for chewing and biting, contributing to proper mastication and facial expressions.
Damage to the mandibular nerve can not only result in sensory loss but also impair the patient’s ability to perform daily activities such as eating and speaking. The loss of sensation in the lower face can lead to difficulties in detecting hot or cold stimuli, increasing the risk of burns or injuries. Furthermore, the loss of motor function can affect the patient’s ability to chew food properly, potentially leading to malnutrition and compromised oral health.
Preserving the integrity of the mandibular nerve during surgical procedures is of utmost importance. Surgeons must exercise caution and employ meticulous techniques to avoid any inadvertent nerve injury. This includes careful identification and protection of the nerve during procedures such as wisdom tooth extraction, dental implant placement, and orthognathic surgeries.
Preoperative imaging techniques, such as cone beam computed tomography (CBCT), can aid in visualizing the course of the mandibular nerve and its relationship to adjacent structures. This information allows surgeons to plan their approach and minimize the risk of nerve injury. Additionally, intraoperative monitoring techniques, such as nerve stimulation and sensory testing, can provide real-time feedback to ensure the safety of the mandibular nerve during surgery.
In conclusion, a comprehensive understanding of the anatomy and importance of the mandibular nerve is crucial for any dental or maxillofacial surgeon. By recognizing the complex course of the nerve and its relationship to surrounding structures, surgeons can minimize the risk of nerve injury and ensure optimal patient outcomes.
Risks of Mandibular Nerve Injury During Surgery
When it comes to surgical procedures involving the mandible, there are inherent risks that need to be carefully considered. One of the most significant risks is mandibular nerve injury, which can have a profound impact on the patient’s postoperative outcome. It is essential for healthcare professionals to be aware of these risks and take necessary precautions to minimize the chances of nerve damage.
Potential Complications of Mandibular Nerve Damage
When the mandibular nerve is injured during surgery, it can lead to a range of complications that can significantly affect the patient’s well-being. One common manifestation of nerve damage is sensory disturbances. These disturbances can manifest as altered touch perception and numbness, causing discomfort and impairing the patient’s ability to chew and articulate speech.
However, the consequences of mandibular nerve injury go beyond sensory deficits. In some cases, patients may experience chronic pain, known as neuropathic pain, which can persist long after the surgical procedure. This debilitating pain can have a profound impact on the patient’s quality of life, affecting their daily activities and overall well-being.
It is crucial to understand the potential complications associated with mandibular nerve damage to emphasize the importance of avoiding such injuries during surgery. By taking necessary precautions and implementing proper surgical techniques, healthcare professionals can minimize patient suffering and improve postoperative outcomes.
Identifying High-Risk Surgical Procedures
While all surgical procedures involving the mandible carry some risk of nerve injury, certain procedures pose a higher risk due to their proximity to the mandibular nerve. Dental implant placement, orthognathic surgery, and mandibular osteotomy are examples of such high-risk procedures.
Dentists and oral surgeons must be well-informed about these high-risk procedures to ensure they take additional precautions during surgery. By understanding the anatomical structures and their proximity to the mandibular nerve, healthcare professionals can implement techniques that minimize the chances of nerve damage.
It is also important for patients to be aware of the risks associated with these procedures. By having open and honest discussions with their healthcare providers, patients can make informed decisions about their treatment options and actively participate in their own care.
In conclusion, the risks of mandibular nerve injury during surgery are significant and can have a profound impact on the patient’s postoperative outcome. By understanding the potential complications and identifying high-risk procedures, healthcare professionals can take necessary precautions to minimize the chances of nerve damage and improve patient outcomes.
Preoperative Planning and Evaluation
Role of Imaging in Identifying Nerve Location
Preoperative planning is crucial in minimizing the risk of mandibular nerve injury. The use of advanced imaging techniques, such as cone-beam computed tomography (CBCT), allows for precise visualization of the mandibular canal and the nerve’s proximity to the surgical site. This information helps the surgeon identify potential challenges and plan for alternative approaches.
By carefully evaluating the imaging results, surgeons can determine the exact location of the mandibular nerve in relation to other anatomical structures. This knowledge enables them to modify their surgical technique and choose the most suitable approach to minimize the risk of nerve injury.
During the preoperative planning phase, the surgeon may also utilize other imaging modalities, such as magnetic resonance imaging (MRI) or ultrasound, to further assess the nerve’s location and potential variations in its course. These additional imaging techniques provide valuable insights into the three-dimensional anatomy of the mandibular nerve, allowing for a more comprehensive evaluation.
Furthermore, advanced imaging technologies, such as virtual surgical planning (VSP), can be employed to create accurate 3D models of the patient’s mandible and surrounding structures. This enables the surgeon to simulate the surgical procedure, identify potential pitfalls, and develop a detailed surgical plan tailored to the patient’s unique anatomy.
Patient History and Risk Assessment
Prior to surgery, a thorough evaluation of the patient’s medical history is crucial in identifying potential risk factors for nerve injury. Medical conditions such as diabetes, neuropathies, and previous nerve injuries increase the patient’s susceptibility to nerve damage. Additionally, certain medications, such as anticoagulants, can affect bleeding and healing, potentially influencing surgical outcomes.
Surgeons should take the time to assess the patient’s overall health and discuss any concerns or underlying conditions that may impact the surgical procedure. In some cases, consultation with a neurologist or oral and maxillofacial surgeon may be necessary to ensure the best possible outcome.
Moreover, a comprehensive risk assessment should include a detailed examination of the patient’s dental and oral health. Factors such as the presence of dental infections, periodontal disease, or previous dental procedures in the surgical area can affect the overall success of the surgery and the risk of nerve injury.
Furthermore, the patient’s lifestyle choices, such as smoking or alcohol consumption, should be taken into consideration as they can impact wound healing and overall surgical outcomes. Surgeons should educate patients about the importance of maintaining good oral hygiene and following postoperative instructions to minimize the risk of complications.
In conclusion, preoperative planning and evaluation play a vital role in minimizing the risk of mandibular nerve injury during surgery. Advanced imaging techniques provide detailed visualization of the nerve’s location, allowing surgeons to modify their approach accordingly. Additionally, a thorough assessment of the patient’s medical history and risk factors helps identify potential challenges and ensures the best possible outcome. By combining these strategies, surgeons can provide safe and effective surgical care for their patients.
Surgical Techniques to Minimize Nerve Damage
Use of Protective Measures During Surgery
During surgical procedures involving the mandible, taking protective measures is essential to prevent nerve injury. Using techniques such as nerve mapping, whereby the surgeon directly visualizes and tracks the nerve’s course, can guide the surgical approach and minimize the risk of accidental damage.
Furthermore, it is crucial for the surgical team to have a comprehensive understanding of the anatomy of the mandibular nerve and its branches. This knowledge allows them to identify potential areas of vulnerability and take appropriate precautions to safeguard the nerve during the procedure. By carefully studying the patient’s preoperative imaging, surgeons can identify any anatomical variations or anomalies that may increase the risk of nerve injury and adjust their surgical plan accordingly.
Additionally, the use of protective barriers, such as nerve shields or retractors, can provide a physical barrier between the surgical instruments and the nerve, reducing the likelihood of direct trauma. These protective measures act as a safeguard, ensuring that the delicate nerve structures remain shielded from inadvertent injury during the surgical manipulation of surrounding tissues.
Surgeons should also exercise caution when inserting screws or other fixation devices near the mandibular canal, as excessive force can lead to nerve compression or injury. By employing gentle and controlled techniques, surgeons can minimize the risk of nerve damage while achieving the desired surgical outcome.
Precision in Surgical Instrumentation
Precision in surgical instrumentation is crucial in preventing nerve injury. Using sharp, properly maintained instruments minimizes the force required for surgical maneuvers and reduces the risk of unintended nerve damage. Surgeons must ensure that their instruments are in optimal condition, with sharp and intact cutting edges, to minimize the risk of tissue trauma.
Furthermore, choosing the appropriate instrument size for the specific procedure helps to maintain surgical accuracy and avoid unnecessary complications. Using instruments that are too large or too small can increase the risk of unintended nerve injury, as they may not provide the necessary precision and control required for delicate surgical maneuvers.
Surgeons should also exercise caution when addressing bony structures surrounding the mandibular nerve. Careful preparation and removal of bone tissue can help to avoid inadvertent nerve trauma. By utilizing meticulous techniques and ensuring adequate visualization throughout the procedure, surgeons can minimize the risk of nerve injury and optimize patient outcomes.
In conclusion, surgical techniques to minimize nerve damage during procedures involving the mandible require the implementation of protective measures and precision in surgical instrumentation. By employing nerve mapping, protective barriers, and careful surgical techniques, surgeons can significantly reduce the risk of nerve injury and enhance patient safety.
Postoperative Care and Monitoring
Postoperative care and monitoring are crucial aspects of the recovery process following surgery. It is essential to provide meticulous care and closely monitor patients to detect and manage any signs of nerve injury promptly.
One of the potential complications that can occur after surgery is mandibular nerve injury. This type of injury can manifest in various ways, including numbness, tingling, or pain in the lower face and chin. Patients should be educated about these potential manifestations so that they can be aware of any changes and promptly report them to their healthcare provider.
Regular follow-up appointments are an integral part of postoperative care. These appointments allow healthcare providers to monitor the patient’s progress and identify any nerve-related complications early on. By closely collaborating with the patient, surgeons can address any concerns and initiate appropriate interventions if necessary.
Signs of Mandibular Nerve Injury Post-Surgery
Following surgery, meticulous postoperative care and monitoring are essential to detect and manage any signs of nerve injury promptly. Patients should be educated about the potential manifestations of nerve damage, such as numbness, tingling, or pain in the lower face and chin.
Monitoring the patient’s progress through regular follow-up appointments allows for the early identification of any nerve-related complications. Close collaboration between the surgeon and the patient ensures that any concerns are promptly addressed and appropriate interventions are initiated.
In addition to numbness, tingling, and pain, other signs of mandibular nerve injury may include muscle weakness or difficulty in moving the lower jaw. These symptoms can significantly impact a patient’s quality of life and may require specialized care and interventions.
It is important to note that the severity and duration of mandibular nerve injury can vary from patient to patient. Some individuals may experience temporary nerve damage that resolves on its own over time, while others may require more extensive treatment and rehabilitation.
Management of Postoperative Complications
In the event of postoperative complications or signs of mandibular nerve injury, it is crucial to provide timely and specialized care. Patients should be encouraged to consult with their surgeon or seek advice from an oral and maxillofacial surgeon, who can provide expert guidance and recommend appropriate interventions.
Treatment options for nerve injuries can include medication, physiotherapy, and in severe cases, surgical interventions. However, it is essential to note that the specific course of action depends on several factors, such as the extent of the injury, underlying conditions, and individual patient characteristics. Therefore, proper management of postoperative complications requires personalized care and an interdisciplinary approach.
When managing postoperative complications, healthcare providers consider not only the physical aspects but also the psychological and emotional well-being of the patient. Nerve injuries can have a significant impact on a person’s daily life, causing discomfort, functional limitations, and emotional distress. Therefore, a comprehensive approach that addresses all these aspects is essential for optimal patient outcomes.
Furthermore, ongoing communication and collaboration between the healthcare team and the patient are vital throughout the management process. This ensures that the patient’s concerns and preferences are taken into account, and decisions regarding treatment and rehabilitation are made collaboratively.
In conclusion, postoperative care and monitoring play a crucial role in detecting and managing complications, such as mandibular nerve injury. By providing meticulous care, educating patients, and offering timely interventions, healthcare providers can optimize patient outcomes and support their overall well-being.
Future Directions in Preventing Nerve Injury
Technological Advancements in Surgical Procedures
Advancements in technology hold great promise in further minimizing the risk of mandibular nerve injury during surgery. Innovative techniques, such as virtual surgical planning and computer-aided navigation, allow for precise preoperative modeling and intraoperative guidance. This technology enhances surgical accuracy and helps avoid potential complications, including nerve damage.
Ongoing Research in Nerve Protection
Research efforts focused on understanding nerve anatomy and function continue to shed light on nerve protection during surgical procedures. Ongoing studies investigate novel techniques, materials, and treatment modalities to further optimize surgical outcomes and reduce the risk of nerve injury.
Although prevention remains the primary goal, advancements in nerve regeneration and repair offer hope for patients who have experienced mandibular nerve injury. Restoring sensory and functional capabilities through emerging regenerative approaches may revolutionize the field and improve the quality of life for affected individuals.
In conclusion, preventing mandibular nerve injury during surgery is a multifaceted process that requires comprehensive understanding, meticulous planning, and precise execution. By prioritizing patient safety, surgeons can minimize the risk of nerve damage and provide optimal outcomes. However, it is essential to emphasize that each case is unique, and individual patient characteristics should guide treatment decisions. Patients should consult with a qualified healthcare professional to address their specific concerns and ensure personalized care.