how many branches does the mandibular nerve have
The mandibular nerve, one of the three branches of the trigeminal nerve, plays a crucial role in innervating the lower half of the face. Understanding the anatomy and function of this nerve is essential for proper diagnosis and management of various pathologies. In this article, we will delve into the intricacies of the mandibular nerve and explore its branches, importance, associated disorders, and common questions surrounding its functioning.
Understanding the Mandibular Nerve
The Role and Function of the Mandibular Nerve
The mandibular nerve, also known as the inferior maxillary nerve, plays a crucial role in the sensory innervation of the face. It is responsible for providing sensory information to a significant portion of the face, including the lower lip, chin, buccal mucosa, lower teeth, and gums. This extensive coverage allows us to perceive touch, temperature, and pain in these areas, enabling us to interact with the world around us.
But the mandibular nerve’s function extends beyond sensory perception. It also innervates the masticatory muscles, which are essential for chewing. These muscles include the masseter, temporalis, medial pterygoid, and lateral pterygoid muscles. By supplying these muscles with motor innervation, the mandibular nerve allows us to perform the complex movements required for biting, chewing, and grinding food.
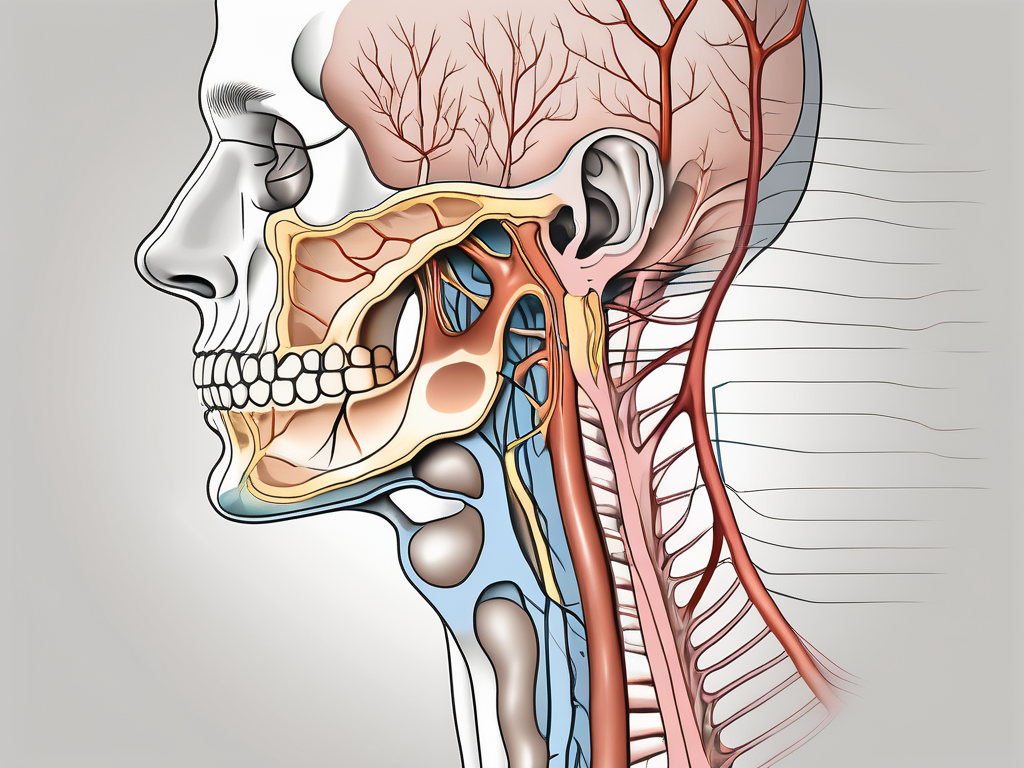
The Anatomy of the Mandibular Nerve
The mandibular nerve originates from the trigeminal ganglion, a collection of nerve cell bodies located within the cranial cavity. This ganglion is one of the three major sensory ganglia of the trigeminal nerve, which is responsible for the sensory innervation of the face.
After its origin, the mandibular nerve courses through the foramen ovale, a bony opening located in the skull. This foramen serves as a passageway for the nerve, allowing it to exit the cranial cavity and enter the infratemporal fossa. The infratemporal fossa is a space located deep within the skull, posterior to the maxilla and lateral to the pterygoid plates.
Once in the infratemporal fossa, the mandibular nerve gives rise to several branches, each with its own distinct pathway and function. These branches include the auriculotemporal nerve, which provides sensory innervation to the temporomandibular joint and the skin of the temple, and the buccal nerve, which supplies sensation to the buccal mucosa and the skin of the cheek.
Another important branch of the mandibular nerve is the inferior alveolar nerve. This nerve travels through the mandibular foramen, a small opening located on the medial surface of the ramus of the mandible. The inferior alveolar nerve supplies sensory innervation to the lower teeth and gums, allowing us to perceive sensations such as pressure, temperature, and pain in this region.
Additionally, the mandibular nerve gives rise to the lingual nerve, which provides sensory innervation to the anterior two-thirds of the tongue. This allows us to taste and perceive sensations such as touch, temperature, and pain on the surface of the tongue.
Understanding the intricate anatomy and function of the mandibular nerve is crucial for dental professionals, as it plays a vital role in dental procedures such as local anesthesia and oral surgery. By comprehending the pathways and branches of this nerve, dental practitioners can ensure effective and precise treatment, minimizing discomfort and maximizing patient care.
The Branches of the Mandibular Nerve
Identifying the Different Branches
The mandibular nerve, also known as the V3 branch of the trigeminal nerve, is a major nerve that provides sensory and motor innervation to the lower face and jaw. It branches into multiple subdivisions, each serving specific regions of the face. These include the auriculotemporal nerve, inferior alveolar nerve, lingual nerve, buccal nerve, and mental nerve. Each of these branches follows a unique trajectory, allowing for precise innervation of the corresponding areas.
The auriculotemporal nerve, one of the branches of the mandibular nerve, supplies sensory fibers to the external ear, temporal region, and skin over the parotid gland. It plays a crucial role in transmitting sensory information from these areas to the brain, allowing us to perceive touch, temperature, and pain.
The inferior alveolar nerve, another branch of the mandibular nerve, provides sensory innervation to the mandibular teeth, lower lip, and chin. It is responsible for transmitting sensations such as touch, pressure, and temperature from these areas to the brain. Additionally, it also carries motor fibers that innervate the muscles responsible for chewing.
The lingual nerve, a significant branch of the mandibular nerve, plays a crucial role in providing taste sensation to the anterior two-thirds of the tongue and a portion of the floor of the mouth. It carries sensory fibers that allow us to perceive different tastes, such as sweet, sour, salty, and bitter. In addition to taste sensation, the lingual nerve also provides general sensory innervation to the tongue, allowing us to perceive touch, temperature, and pain.
The buccal nerve, another branch of the mandibular nerve, innervates the buccal mucosa and the skin of the cheek. It carries sensory fibers that transmit touch, pressure, and temperature sensations from these areas to the brain. The buccal nerve also plays a role in transmitting pain sensations, allowing us to perceive discomfort or injury in the cheek region.
Lastly, the mental nerve, a branch of the inferior alveolar nerve, supplies sensory fibers to the skin of the chin and lower lip. It carries sensory information related to touch, pressure, temperature, and pain from these areas to the brain. The mental nerve is responsible for our ability to perceive sensations in the chin and lower lip region.
The Purpose of Each Branch
The branches of the mandibular nerve serve crucial functions in the sensory and motor innervation of the face. Understanding the purpose of each branch provides insight into the complex network of nerves that allow us to perceive and interact with our environment.
The auriculotemporal nerve, with its sensory fibers to the external ear, temporal region, and skin over the parotid gland, enables us to feel touch, temperature, and pain in these areas. It plays a role in our ability to hear and perceive sound, as well as providing sensory feedback from the skin over the parotid gland.
The inferior alveolar nerve, with its sensory innervation to the mandibular teeth, lower lip, and chin, allows us to perceive sensations related to touch, pressure, and temperature in these areas. It also carries motor fibers that control the muscles responsible for chewing, enabling us to bite and chew our food effectively.
The lingual nerve, responsible for taste sensation in the anterior two-thirds of the tongue and a portion of the floor of the mouth, allows us to enjoy the flavors of different foods. It also provides general sensory innervation to the tongue, allowing us to perceive touch, temperature, and pain, which are essential for speech and swallowing.
The buccal nerve, innervating the buccal mucosa and the skin of the cheek, plays a role in our ability to perceive touch, pressure, and temperature in these areas. It also carries pain fibers, allowing us to detect and respond to potential injuries or irritations in the cheek region.
The mental nerve, supplying sensory fibers to the skin of the chin and lower lip, enables us to perceive touch, pressure, temperature, and pain in these areas. It is responsible for our ability to feel sensations related to the chin and lower lip, providing important feedback for activities such as speaking, eating, and facial expressions.
The Importance of the Mandibular Nerve Branches
How the Branches Affect Facial Sensation
Understanding the branches of the mandibular nerve is of paramount importance in diagnosing and managing potential issues related to facial sensation. The mandibular nerve, a major branch of the trigeminal nerve, plays a crucial role in providing sensory innervation to various areas of the face. It is responsible for transmitting sensations such as touch, temperature, and pain from the lower jaw, lower teeth, and the skin of the chin.
Within the mandibular nerve, there are several branches that supply different regions of the face. These branches include the inferior alveolar nerve, the mental nerve, and the buccal nerve. Each branch has its own specific distribution and function, contributing to the overall sensory perception of the face.
For example, in cases of trauma or dental procedures involving the inferior dental nerve, careful consideration must be given to preserve its function to prevent transient or permanent numbness in the innervated areas. The inferior dental nerve, a branch of the mandibular nerve, provides sensory innervation to the lower teeth and gums. Any damage to this nerve can result in altered sensation or complete numbness in the affected area, leading to difficulties in chewing, speaking, and overall oral health.
The Mandibular Nerve and Dental Procedures
Dental professionals must be well-versed in the anatomy of the mandibular nerve and its branches to ensure the safe administration of local anesthesia. Proper knowledge and technique can help minimize the risk of nerve injury and subsequent sensory disturbances in dental procedures such as extractions, root canals, and implant placements.
During dental procedures, local anesthesia is commonly used to numb the area being treated, providing comfort and pain relief to the patient. The administration of local anesthesia requires precise placement of the anesthetic agent near the targeted nerve branches. Understanding the course and distribution of the mandibular nerve branches is crucial in achieving effective anesthesia while minimizing the risk of nerve damage.
In cases where patients experience prolonged or abnormal sensations following dental procedures, consulting with a healthcare professional is recommended. Sensory disturbances, such as tingling, numbness, or hypersensitivity, may occur due to various factors, including nerve irritation, inflammation, or temporary nerve dysfunction. Prompt evaluation and appropriate management can help alleviate these symptoms and ensure optimal recovery.
In conclusion, the branches of the mandibular nerve play a vital role in facial sensation. Dental professionals must have a comprehensive understanding of the anatomy and function of these branches to ensure safe and effective dental procedures. By prioritizing the preservation of nerve function and promptly addressing any sensory disturbances, healthcare providers can optimize patient care and outcomes.
Disorders Related to the Mandibular Nerve
The mandibular nerve is a branch of the trigeminal nerve, which is responsible for providing sensory innervation to the lower face and jaw. Disorders related to the mandibular nerve can manifest in various ways, causing discomfort and affecting daily activities.
Symptoms of Mandibular Nerve Disorders
When the mandibular nerve is affected, individuals may experience a range of symptoms. One of the most common symptoms is facial pain, which can be dull, throbbing, or sharp in nature. This pain may radiate to the jaw, ear, or temple, making it difficult to pinpoint the exact source.
In addition to facial pain, individuals may also experience numbness or tingling in the lower face and chin. This altered sensation can be unsettling and may affect the ability to feel touch or temperature changes in the affected areas.
Another symptom of mandibular nerve disorders is altered sensation in the tongue. Individuals may notice a tingling or “pins and needles” sensation in the tongue, making it uncomfortable to eat or speak. This can significantly impact one’s quality of life and ability to communicate effectively.
Difficulties with chewing or speaking are also common symptoms of mandibular nerve disorders. The mandibular nerve plays a crucial role in the movement and coordination of the muscles involved in chewing and speaking. When the nerve is affected, individuals may experience weakness, difficulty controlling their jaw movements, or slurred speech.
It is important to note that while these symptoms are commonly associated with mandibular nerve disorders, they can also arise from other underlying health conditions. Therefore, consulting with a healthcare professional for proper evaluation and diagnosis is crucial. A thorough examination, including a detailed medical history and possibly imaging studies, may be necessary to determine the exact cause of the symptoms.
Treatment Options for Mandibular Nerve Disorders
The treatment strategies for mandibular nerve disorders depend on the underlying cause and severity of the condition. In many cases, conservative approaches are considered as the first line of therapy.
Pain management techniques, such as applying heat or cold packs to the affected area, can help alleviate facial pain. Physical therapy may also be recommended to improve jaw mobility and strengthen the muscles involved in chewing and speaking. Additionally, medications, such as nonsteroidal anti-inflammatory drugs (NSAIDs) or anticonvulsants, may be prescribed to manage pain and reduce nerve-related symptoms.
In severe cases or when conservative measures fail to provide relief, surgical interventions may be explored. Surgical options for mandibular nerve disorders aim to alleviate symptoms and restore normal function. Procedures such as nerve decompression, nerve grafting, or nerve repair may be considered, depending on the specific condition and individual needs.
It is important to note that the treatment plan will be tailored to each individual after a comprehensive evaluation by a healthcare professional. The underlying cause, severity of symptoms, and individual preferences will all be taken into consideration when determining the most appropriate course of action.
In conclusion, disorders related to the mandibular nerve can cause a range of symptoms, including facial pain, numbness or tingling in the lower face and chin, altered sensation in the tongue, and difficulties with chewing or speaking. Seeking proper evaluation and diagnosis from a healthcare professional is essential for effective management and treatment. With the right approach, individuals can find relief and regain normal function, improving their overall quality of life.
Frequently Asked Questions about the Mandibular Nerve
The mandibular nerve is a crucial component of the trigeminal nerve, which is responsible for providing sensory innervation to the face. It is the largest of the three branches of the trigeminal nerve and plays a vital role in facilitating chewing and providing sensation to the lower jaw, teeth, and gums.
Common Misconceptions about the Mandibular Nerve
There are some common misconceptions regarding the mandibular nerve. One such misconception is that it can spontaneously regenerate following injury. However, the regenerative capacity of the nerve is limited, and in cases of severe injury, full recovery may be challenging. It is important to understand the potential limitations and manage expectations when it comes to nerve injuries and recovery.
Another misconception is that the mandibular nerve is solely responsible for dental pain. While it does provide sensory innervation to the teeth and gums, other nerves, such as the maxillary nerve, also contribute to dental sensation. Therefore, it is essential to consider a comprehensive approach when diagnosing and treating dental pain.
The Future of Mandibular Nerve Research
Ongoing research in the field of neuroscience focuses on gaining deeper insights into the molecular mechanisms and regenerative potential of nerves, including the mandibular nerve. Scientists are exploring various strategies to enhance nerve regeneration and functional recovery, such as the use of growth factors, stem cells, and tissue engineering techniques.
Additionally, researchers are investigating the role of neurotrophic factors, which are proteins that support the growth and survival of nerve cells. By understanding how these factors influence the mandibular nerve’s regenerative capacity, scientists hope to develop targeted therapies that can promote nerve repair and improve outcomes for patients with nerve injuries or damage.
Furthermore, advancements in imaging technology, such as high-resolution magnetic resonance imaging (MRI) and diffusion tensor imaging (DTI), are enabling researchers to visualize the intricate pathways and connections of the mandibular nerve in greater detail. This improved understanding of the nerve’s anatomy can aid in surgical planning and improve outcomes for procedures involving the mandibular nerve.
In conclusion, the mandibular nerve branches intricately throughout the face, providing vital sensory innervation and facilitating chewing. Understanding the anatomy, function, and potential disorders associated with these branches is crucial for dental professionals and individuals experiencing related symptoms. If you have concerns or symptoms related to the mandibular nerve, it is advised to seek the expertise of a healthcare professional for proper evaluation and guidance.