how to avoid marginal mandibular nerve injury “notch”
The marginal mandibular nerve is a crucial nerve located in the face. It plays a significant role in controlling the movement and function of the lower lip, chin, and corners of the mouth. Despite its importance, this nerve can be susceptible to injury, leading to a condition commonly referred to as the “notch.” This article aims to shed light on the anatomy, causes, symptoms, and preventive measures related to marginal mandibular nerve injury, as well as treatment options and the impact it can have on an individual’s quality of life.
Understanding the Marginal Mandibular Nerve
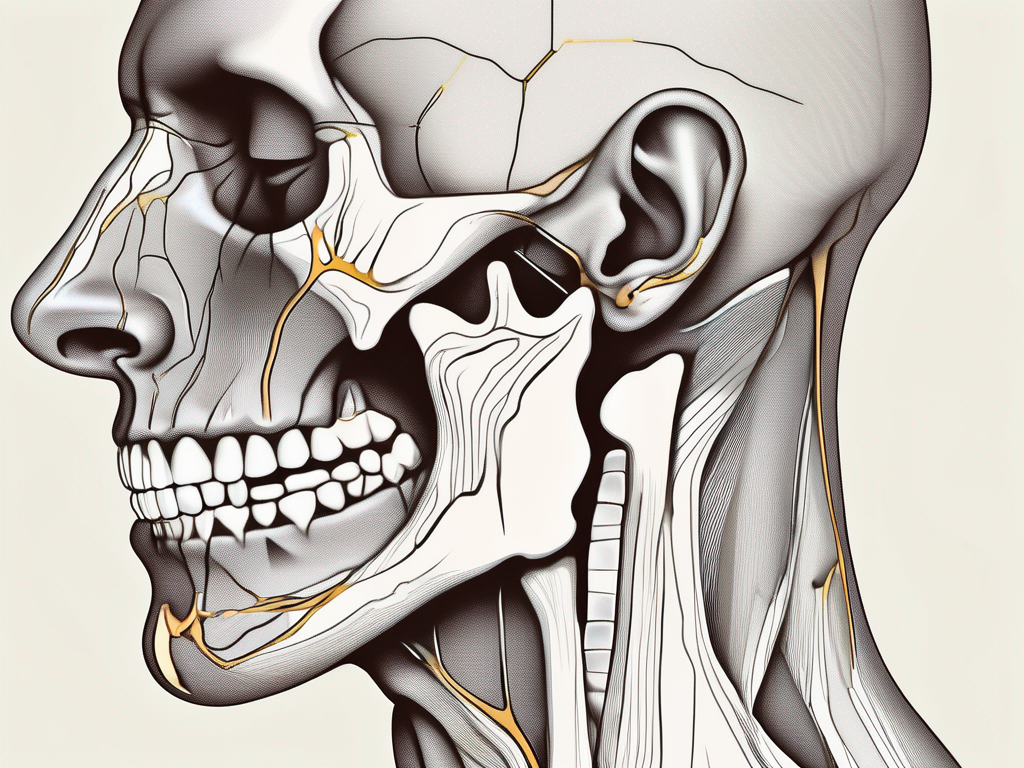
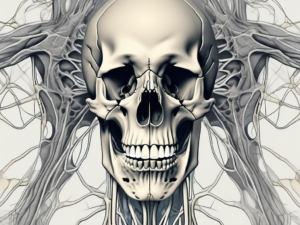
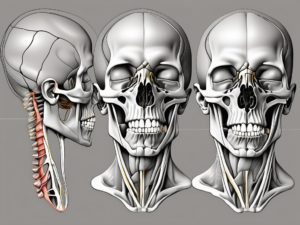
Before delving into the specifics of avoiding marginal mandibular nerve injury, it is essential to comprehend the underlying anatomy and function of this nerve. The marginal mandibular nerve is a branch of the facial nerve, originating in the brainstem and extending through the face. It runs a course that is parallel to the mandible’s lower border, hence its name.
The primary function of the marginal mandibular nerve is to innervate the muscles responsible for controlling the lower lip and chin, allowing for facial expressions, speaking, and swallowing. Any damage to this nerve can lead to significant impairments in these functions, impacting a person’s overall quality of life.
Anatomy of the Marginal Mandibular Nerve
The marginal mandibular nerve is typically found at the level of the mandible’s lower border, slightly above the chin region. It travels in close proximity to vital structures, including blood vessels and other nerves. Understanding the precise anatomical landmarks and variations is crucial for avoiding inadvertent injury during surgical procedures or other related interventions.
When examining the anatomy of the marginal mandibular nerve, it is important to note its relationship with the surrounding structures. The nerve often lies just beneath the platysma muscle, a thin sheet of muscle that covers the front of the neck. This close proximity can make the nerve vulnerable to injury during surgical procedures that involve the neck or lower face.
Additionally, the marginal mandibular nerve may have variations in its course and branching patterns. While the nerve typically runs parallel to the mandible’s lower border, there can be variations in its exact path. Surgeons and medical professionals must be aware of these variations to ensure the safe and effective management of patients.
Function of the Marginal Mandibular Nerve
As mentioned earlier, the marginal mandibular nerve primarily innervates specific muscles that control the lower lip and chin movements. It ensures proper oral competence, allowing for various activities such as articulating speech sounds, consuming food, and maintaining facial expressions. The intricate interplay between this nerve and the surrounding structures allows for seamless coordination and function of the lower face.
When the marginal mandibular nerve is functioning properly, it allows for precise control of the lower lip and chin muscles. This control is essential for activities such as smiling, pouting, and forming words. The nerve works in conjunction with other facial nerves to create a symphony of movements that give the face its unique expressions.
However, when the marginal mandibular nerve is damaged or injured, it can result in a condition known as marginal mandibular nerve palsy. This condition can cause weakness or paralysis of the lower lip and chin muscles, leading to difficulties in speaking, eating, and even drooling. The impact on a person’s self-esteem and quality of life can be significant, making it crucial to avoid injury to this vital nerve.
Causes of Marginal Mandibular Nerve Injury
There are various factors that can contribute to marginal mandibular nerve injury. Understanding these causes can help individuals and healthcare professionals avoid potential harm and implement preventive strategies.
The marginal mandibular nerve, also known as the marginal mandibular branch of the facial nerve, is a crucial nerve that innervates the muscles of the lower lip and chin. Any damage to this nerve can result in significant functional and aesthetic consequences.
Surgical Procedures and Risks
Marginal mandibular nerve injury can occur during surgical procedures involving the lower face, chin, or neck region. Plastic surgery interventions such as facelifts or aesthetic procedures targeting the mandibular area carry a certain risk of nerve damage. The complexity of these procedures, the proximity of the nerve to the surgical site, and the delicate nature of the nerve itself contribute to the potential for injury.
However, it is crucial to note that these risks vary depending on the surgeon’s expertise, patient characteristics, and the specific techniques employed. Experienced surgeons who prioritize patient safety and take necessary precautions can significantly reduce the likelihood of nerve injury. Individuals considering such procedures should thoroughly discuss the potential complications, including nerve injury, with their healthcare provider to make informed decisions.
In some cases, nerve injuries during surgical procedures may be temporary, with the nerve regenerating and restoring function over time. However, in more severe cases, permanent damage can occur, leading to long-term functional and aesthetic impairments.
Non-Surgical Causes of Injury
While surgical procedures pose a significant risk, it is essential to recognize that non-surgical causes can also contribute to marginal mandibular nerve injury. Traumatic events, such as accidental trauma to the face or head, can lead to nerve damage. Impact from falls, sports injuries, or motor vehicle accidents can exert excessive force on the nerve, resulting in injury.
Additionally, prolonged pressure or compression on the nerve can increase the likelihood of injury. Ill-fitting dental appliances, such as braces or dentures, can exert constant pressure on the nerve, leading to nerve compression and potential damage. Similarly, individuals who regularly wear masks for extended periods, such as healthcare professionals or individuals in certain occupational settings, may experience nerve injury due to prolonged pressure on the nerve.
Identifying and addressing these non-surgical risk factors is crucial for minimizing the chances of marginal mandibular nerve injury. Proper fitting of dental appliances, regular check-ups with healthcare providers, and taking necessary precautions to prevent accidental trauma can all contribute to maintaining the health and integrity of the nerve.
In conclusion, understanding the causes of marginal mandibular nerve injury is essential for both individuals and healthcare professionals. By being aware of the potential risks associated with surgical procedures and non-surgical factors, individuals can make informed decisions and take necessary precautions to protect the nerve and minimize the chances of injury.
Symptoms and Diagnosis of Marginal Mandibular Nerve Injury
Recognizing the symptoms associated with marginal mandibular nerve injury is vital for early intervention and management. Prompt diagnosis allows healthcare professionals to develop a comprehensive treatment plan tailored to the individual’s needs.
When it comes to marginal mandibular nerve injury, understanding the symptoms is crucial. These symptoms often manifest in distinct ways, providing important clues for diagnosis and treatment. One of the most common signs is the drooping of the lower lip on the affected side. This drooping can be quite noticeable and may affect speech and eating. Additionally, individuals may experience difficulty with lip and chin movements, making it challenging to perform everyday tasks such as smiling or chewing. Another telltale symptom is the asymmetry of facial expressions, where one side of the face appears different from the other. These symptoms, when present, should not be ignored, as they could be indicative of a marginal mandibular nerve injury.
Recognizing the Symptoms
Marginal mandibular nerve injury often presents with characteristic symptoms. These may include drooping of the lower lip on the affected side, difficulty with lip and chin movements, and asymmetry of facial expressions. When experiencing such symptoms, it is crucial to consult with a healthcare professional for a thorough evaluation and appropriate diagnosis.
When it comes to recognizing the symptoms of marginal mandibular nerve injury, it is important to pay attention to subtle changes in facial appearance and function. The drooping of the lower lip can make it difficult to maintain a normal smile, and it may even affect the ability to speak clearly. Lip and chin movements can become impaired, leading to challenges in performing everyday activities like eating or applying makeup. The asymmetry of facial expressions can be emotionally distressing, as it alters the overall appearance of the face. These symptoms, though they may seem minor at first, should not be ignored, as they can indicate a more significant underlying issue.
Diagnostic Procedures
Healthcare professionals employ various diagnostic procedures to confirm marginal mandibular nerve injury. These may include detailed physical examinations, electromyography (EMG) to assess nerve function, and imaging techniques to visualize the nerve and surrounding structures. Consulting with a healthcare professional is essential to determine the most appropriate diagnostic approach based on individual circumstances.
When it comes to diagnosing marginal mandibular nerve injury, healthcare professionals utilize a range of diagnostic procedures to ensure accurate assessment and treatment planning. A detailed physical examination is often the first step, where the healthcare provider carefully evaluates the patient’s facial movements, muscle strength, and overall facial symmetry. This examination helps to identify any abnormalities or weaknesses that may be indicative of nerve injury.
In addition to the physical examination, electromyography (EMG) is commonly used to assess nerve function. During an EMG, small electrodes are placed on the skin to measure the electrical activity of the muscles controlled by the marginal mandibular nerve. This test provides valuable information about the nerve’s health and functionality.
Imaging techniques, such as magnetic resonance imaging (MRI) or computed tomography (CT) scans, may also be employed to visualize the nerve and surrounding structures in more detail. These imaging modalities can help identify any structural abnormalities or potential causes of the nerve injury.
It is important to note that the specific diagnostic approach may vary depending on the individual’s symptoms, medical history, and the healthcare professional’s expertise. Therefore, consulting with a healthcare professional is essential to determine the most appropriate diagnostic procedures for each unique case.
Preventive Measures for Marginal Mandibular Nerve Injury
In many cases, marginal mandibular nerve injury is avoidable with proper planning and precautionary strategies. Whether considering surgical interventions or aiming to reduce non-surgical risk factors, preventive measures can help minimize the likelihood of nerve injury.
Pre-Surgical Planning and Techniques
For individuals undergoing surgical procedures involving the lower face, meticulous pre-operative planning and a surgeon skilled in the anatomy of the marginal mandibular nerve are essential. Detailed discussions with the surgeon beforehand allow patients to understand the potential risks involved and the steps taken to prevent nerve injury. Proper surgical techniques, such as gentle tissue handling and careful incision placement, can significantly reduce the likelihood of any inadvertent nerve damage.
In addition to these measures, there are other aspects of pre-surgical planning that can contribute to the prevention of marginal mandibular nerve injury. These include conducting thorough pre-operative assessments to identify any pre-existing conditions or anatomical variations that may increase the risk of nerve injury. By identifying these factors in advance, surgeons can develop personalized strategies to minimize the chances of nerve damage during the procedure.
Furthermore, the use of advanced imaging techniques, such as magnetic resonance imaging (MRI) or computed tomography (CT) scans, can provide surgeons with detailed anatomical information. This allows for precise identification and mapping of the marginal mandibular nerve, enabling surgeons to navigate around it with greater accuracy during the surgical procedure.
Non-Surgical Prevention Strategies
When looking to minimize the chances of non-surgical marginal mandibular nerve injury, individuals can adopt various preventive strategies. This includes ensuring proper fitting of dental appliances, employing appropriate protective equipment in high-risk activities, and regularly reassessing prolonged pressure points on the lower face. Consulting with healthcare professionals, such as dentists or occupational therapists, can provide valuable guidance in implementing these preventive measures.
In addition to these strategies, maintaining good overall health and practicing proper oral hygiene can also contribute to the prevention of marginal mandibular nerve injury. Regular dental check-ups and cleanings can help identify any potential issues that may increase the risk of nerve injury, allowing for early intervention and preventive measures.
Furthermore, individuals engaging in activities that pose a higher risk of facial trauma, such as contact sports or certain occupations, should consider using appropriate protective equipment. This can include mouthguards, face shields, or helmets, depending on the specific activity. By taking these precautions, the risk of accidental trauma to the marginal mandibular nerve can be significantly reduced.
Lastly, individuals who regularly experience prolonged pressure points on the lower face, such as those who wear tight-fitting masks or headgear for extended periods, should make a conscious effort to reassess and relieve these pressure points regularly. This can be achieved by adjusting the fit of the equipment, taking breaks to remove the pressure, or using padding to distribute the force more evenly. By relieving these pressure points, the risk of nerve injury due to compression or ischemia can be minimized.
Treatment Options for Marginal Mandibular Nerve Injury
While prevention is crucial, marginal mandibular nerve injury can still occur despite best efforts. In such cases, understanding the available treatment options is vital for effective management.
Marginal mandibular nerve injury can result from various causes, including trauma, surgical procedures, or underlying medical conditions. The severity of the nerve damage and the specific symptoms experienced by the individual will determine the most appropriate treatment approach.
Immediate Interventions
Immediate interventions for marginal mandibular nerve injury depend on the severity and underlying cause of the nerve damage. In some cases, conservative approaches, such as observation or physical therapy, may be sufficient to allow nerve healing and recovery.
Observation involves closely monitoring the progression of symptoms and providing supportive care while waiting for the nerve to heal on its own. Physical therapy can help improve muscle strength and coordination, as well as promote nerve regeneration through targeted exercises and techniques.
However, more severe cases may necessitate surgical interventions to repair or graft the damaged nerve. Nerve repair involves reconnecting the damaged ends of the nerve, while nerve grafting involves using a section of nerve from another part of the body to bridge the gap and facilitate regeneration.
It is important to consult with knowledgeable healthcare professionals, such as neurologists or oral and maxillofacial surgeons, to determine the most appropriate immediate interventions for individual circumstances. They will consider factors such as the extent of the nerve injury, the individual’s overall health, and the potential risks and benefits of each treatment option.
Long-Term Management and Rehabilitation
Long-term management following marginal mandibular nerve injury often involves a multidisciplinary approach. This may include ongoing physical therapy to maintain muscle strength and mobility, speech therapy to address any speech-related difficulties, and psychological support to manage potential emotional implications.
Physical therapy plays a crucial role in the rehabilitation process by helping individuals regain normal muscle function and control. Therapists may use a variety of techniques, such as exercises, manual therapy, and electrical stimulation, to stimulate nerve regeneration and improve overall oral function.
Speech therapy focuses on addressing any speech-related difficulties that may arise from the nerve injury. Therapists work with individuals to improve articulation, voice projection, and swallowing abilities, ensuring effective communication and minimizing any functional limitations.
Psychological support is also an essential component of long-term management. Coping with the physical and emotional challenges of a marginal mandibular nerve injury can be overwhelming for individuals. Mental health professionals can provide guidance, counseling, and support to help individuals navigate through the recovery process and maintain a positive outlook.
Collaborating with a team of healthcare professionals, including neurologists, oral and maxillofacial surgeons, physical therapists, speech-language pathologists, and mental health professionals, can aid in optimizing long-term outcomes. This multidisciplinary approach ensures that all aspects of the individual’s well-being are addressed, leading to a comprehensive and effective treatment plan.
The Impact of Marginal Mandibular Nerve Injury on Quality of Life
Marginal mandibular nerve injury can have significant implications on an individual’s quality of life. Understanding the physical, psychological, and social consequences is crucial for comprehensive care and support.
Physical Implications
The physical impact of marginal mandibular nerve injury can range from mild functional limitations to more severe difficulties with facial expressions, speech, and swallowing. These physical changes can affect self-esteem, social interactions, and daily activities. Seeking appropriate interventions and support can aid in managing these physical implications and promoting overall well-being.
Psychological and Social Implications
Individuals affected by marginal mandibular nerve injury may experience various psychological and social challenges. Changes in facial appearance or the ability to communicate effectively can lead to decreased self-confidence, isolation, and an altered self-image. Seeking professional psychological support and engaging in support networks can assist individuals in navigating these challenges and fostering resilience.
In conclusion, understanding how to avoid marginal mandibular nerve injury is crucial for both healthcare professionals and individuals. By comprehending the anatomy, recognizing the causes and symptoms, implementing preventive measures, and exploring the available treatment options, one can minimize the risks associated with this condition. Collaborating with healthcare professionals and seeking their expertise is essential for tailored care and optimal outcomes. Prioritizing the well-being of the marginal mandibular nerve can contribute to maintaining a healthy and fulfilling life.