why does my mandibular nerve hurt
The mandibular nerve, also known as the inferior alveolar nerve, is a crucial component of the trigeminal nerve, which is responsible for sensation in the face. When this nerve is affected, it can lead to significant discomfort and pain. Understanding the causes, symptoms, diagnostic procedures, treatment options, and prevention strategies for mandibular nerve pain is essential for individuals experiencing this condition. In this article, we will delve into the intricate details of mandibular nerve pain, providing valuable insights that can help shed light on this perplexing issue.
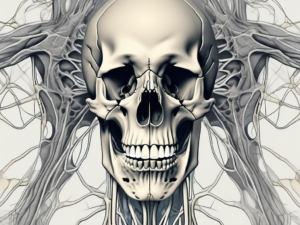
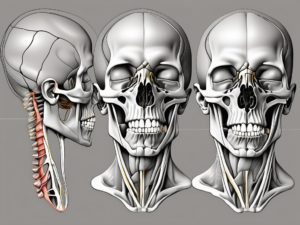
Understanding the Mandibular Nerve
The mandibular nerve is a crucial component of the trigeminal nerve, which is responsible for providing sensory information from the face to the brain. It is the largest of the three branches of the trigeminal nerve and has a complex anatomy.
Anatomy of the Mandibular Nerve
The mandibular nerve originates from the trigeminal ganglion, a cluster of nerve cell bodies located deep within the skull. From there, it travels posteriorly, passing through the foramen ovale, a bony opening in the skull. As it exits the skull, the mandibular nerve divides into several branches, each with its own specific function.
One of the main branches of the mandibular nerve is the inferior alveolar nerve. This nerve supplies sensation to the lower teeth and gums. It travels through the mandibular canal, a tunnel-like structure within the lower jawbone, before branching out to innervate the teeth and surrounding tissues.
Another important branch of the mandibular nerve is the mental nerve. This nerve provides sensation to the chin and lower lip. It emerges from the mental foramen, a small opening in the lower jawbone, and distributes sensory fibers to the skin and mucous membranes of the chin and lower lip.
In addition to these branches, the mandibular nerve also gives rise to the buccal nerve, which supplies sensation to the cheek, and the lingual nerve, which provides sensory innervation to the anterior two-thirds of the tongue.
Function of the Mandibular Nerve
The primary function of the mandibular nerve is to provide sensory innervation to the lower face. It carries information about touch, temperature, and pain from the skin, teeth, and mucous membranes of the lower jaw, chin, lips, and part of the tongue.
Furthermore, the mandibular nerve plays a vital role in controlling the muscles responsible for chewing and biting. It innervates the muscles of mastication, including the masseter, temporalis, and lateral pterygoid muscles. These muscles work together to move the jaw during chewing and biting, allowing us to break down food into smaller, more digestible pieces.
Damage or dysfunction of the mandibular nerve can lead to various symptoms and conditions. For example, injury to the inferior alveolar nerve can result in numbness or tingling in the lower teeth and gums, while damage to the mental nerve can cause altered sensation in the chin and lower lip.
In summary, the mandibular nerve is a crucial component of the trigeminal nerve, responsible for providing sensory innervation to the lower face and controlling the muscles of mastication. Its complex anatomy and important functions make it an essential part of our ability to eat, speak, and experience sensation in the lower part of our face.
Common Causes of Mandibular Nerve Pain
Dental Issues and Mandibular Nerve Pain
One of the most prevalent causes of mandibular nerve pain is dental problems. In cases of dental abscesses, impacted wisdom teeth, or dental procedures gone wrong, irritation or inflammation of the mandibular nerve may occur. It is imperative to note that any dental issues should be promptly addressed by a qualified dentist. Seeking professional dental care can help alleviate or prevent potential mandibular nerve pain.
Dental abscesses, which are localized infections in the teeth or gums, can cause excruciating pain that radiates to the mandibular nerve. The infection can spread and affect the surrounding tissues, leading to further inflammation and nerve irritation. Prompt treatment, such as root canal therapy or tooth extraction, may be necessary to resolve the abscess and relieve the associated nerve pain.
Impacted wisdom teeth, also known as third molars, can exert pressure on the surrounding nerves, including the mandibular nerve. This pressure can cause pain, numbness, and tingling sensations in the jaw, face, and even the neck. Surgical extraction of the impacted wisdom teeth is often recommended to alleviate the nerve compression and eliminate the source of pain.
While dental procedures are generally safe, complications can sometimes arise, leading to mandibular nerve pain. Nerve damage can occur during tooth extractions, dental implants, or root canal treatments, especially if the dentist is inexperienced or if there are anatomical variations in the nerve’s pathway. In such cases, seeking immediate medical attention and consulting with a specialist, such as an oral and maxillofacial surgeon, may be necessary to address the nerve injury and minimize long-term pain.
Trauma and the Mandibular Nerve
Physical trauma, such as accidents or sports injuries, can have a significant impact on the mandibular nerve. Direct blows to the face or jaw may result in nerve compression, stretching, or damage. Individuals who have experienced facial trauma should seek immediate medical attention to assess any potential damage to the mandibular nerve.
Motor vehicle accidents can cause severe facial trauma, leading to fractures of the jawbone and potential injury to the mandibular nerve. The force of the impact can compress or stretch the nerve, causing pain, numbness, or even paralysis in the affected area. In such cases, a multidisciplinary approach involving oral and maxillofacial surgeons, neurologists, and physical therapists may be necessary to manage the nerve damage and facilitate recovery.
Sports-related injuries, particularly in contact sports like boxing or rugby, can also result in mandibular nerve pain. A forceful punch or tackle to the jaw can cause nerve compression or damage, leading to persistent discomfort. Athletes who engage in high-risk sports should wear appropriate protective gear, such as mouthguards, to reduce the risk of mandibular nerve injuries.
Infections Impacting the Mandibular Nerve
Infections, such as sinusitis or otitis media, can lead to mandibular nerve pain. Inflammatory processes in the surrounding structures can cause nerve irritation and subsequent discomfort. If you suspect an infection is contributing to your mandibular nerve pain, consulting with a healthcare professional is strongly advised.
Sinusitis, an inflammation of the sinuses, can cause referred pain to the mandibular nerve. The sinuses are located close to the jawbone, and when infected, the inflammation can spread to the nearby nerves, including the mandibular nerve. Symptoms may include facial pain, pressure, and aching in the jaw, which can be mistaken for dental issues. Proper diagnosis and treatment of the underlying sinus infection are crucial to alleviate the associated mandibular nerve pain.
Otitis media, an infection of the middle ear, can also lead to mandibular nerve pain. The middle ear is connected to the temporomandibular joint (TMJ) by a small canal, and infections in this area can spread to the surrounding structures, including the mandibular nerve. The pain may be accompanied by earache, jaw discomfort, and difficulty in opening or closing the mouth. Prompt medical attention and appropriate antibiotic treatment are necessary to resolve the infection and relieve the nerve-related symptoms.
In conclusion, mandibular nerve pain can have various causes, including dental issues, trauma, and infections. Prompt diagnosis and appropriate treatment are essential to alleviate the pain and prevent further complications. If you are experiencing mandibular nerve pain, it is recommended to consult with a healthcare professional or dental specialist for a thorough evaluation and personalized treatment plan.
Symptoms Associated with Mandibular Nerve Pain
Physical Symptoms
The physical symptoms of mandibular nerve pain can vary but often include sharp or shooting pain in the lower face, jaw, or teeth. This pain can be intense, making it difficult for individuals to carry out their daily activities. The pain may radiate from the jaw to the ear or temple, causing discomfort and making it challenging to focus on tasks at hand.
In addition to the pain, individuals with mandibular nerve pain may experience numbness or tingling sensations in the affected areas. This can be particularly bothersome, as it may cause a loss of sensitivity or a “pins and needles” feeling, making it uncomfortable to eat or speak.
Furthermore, mandibular nerve pain can lead to difficulty in opening or closing the mouth and chewing. This can significantly impact an individual’s ability to enjoy meals and can even lead to unintentional weight loss if the pain persists and affects their ability to eat properly.
Overall, these physical symptoms can have a profound impact on an individual’s quality of life. The constant pain and discomfort can make it challenging to engage in social activities, concentrate at work or school, and even perform simple tasks like brushing teeth or talking.
Emotional and Psychological Symptoms
Mandibular nerve pain can also take a toll on an individual’s emotional and psychological well-being. The persistent pain and discomfort can lead to feelings of frustration, helplessness, and even depression. Dealing with chronic pain can be mentally exhausting, and individuals may find themselves constantly worrying about when the next flare-up will occur or how they will manage their pain.
Furthermore, the impact of mandibular nerve pain on daily activities and social interactions can lead to increased anxiety. Individuals may feel self-conscious about their appearance or worry about being misunderstood when they have difficulty speaking or eating in public. This can lead to social isolation and a decrease in self-esteem.
Sleep disturbances are also common among individuals with mandibular nerve pain. The constant pain and discomfort can make it difficult to fall asleep or stay asleep throughout the night. This lack of quality sleep can further exacerbate emotional symptoms, leaving individuals feeling fatigued, irritable, and unable to cope with their pain effectively.
It is crucial to address these emotional symptoms and seek support from healthcare professionals or support groups specializing in chronic pain management. By addressing the emotional and psychological impact of mandibular nerve pain, individuals can develop coping strategies, receive appropriate treatment, and improve their overall well-being.
Diagnostic Procedures for Mandibular Nerve Pain
Medical History and Physical Examination
Diagnosing the cause of mandibular nerve pain often starts with a comprehensive medical history and physical examination. Your healthcare provider will inquire about your symptoms, medical history, and any recent injuries or infections. They will then perform a physical examination, assessing the jaw and surrounding structures for any signs of inflammation or abnormalities.
During the medical history portion of the diagnostic process, your healthcare provider will ask you detailed questions about your symptoms. They will want to know when the pain started, how long it has been going on, and if anything seems to trigger or worsen the pain. Additionally, they will ask about any other symptoms you may be experiencing, such as numbness or tingling in the face or difficulty chewing.
Furthermore, your healthcare provider will inquire about your medical history to identify any pre-existing conditions that may contribute to the mandibular nerve pain. They will also ask about any recent injuries or infections that could potentially be related to the pain.
After gathering the necessary information from the medical history, your healthcare provider will proceed with a physical examination. They will carefully examine your jaw and surrounding structures, looking for any visible signs of inflammation, swelling, or abnormalities. They may gently palpate the affected area to assess for tenderness or pain.
In addition to examining the jaw, your healthcare provider may also evaluate other areas that can contribute to mandibular nerve pain. This may include examining the teeth and gums for signs of dental issues, such as cavities or gum disease. They may also assess the temporomandibular joint (TMJ) for any dysfunction or misalignment that could be causing or exacerbating the pain.
Imaging Tests for Mandibular Nerve Pain
In some cases, imaging tests such as X-rays, CT scans, or MRI scans may be necessary to evaluate the condition of the mandibular nerve. These imaging techniques can provide detailed images of the nerve and surrounding structures, helping identify potential causes of pain or damage.
X-rays are commonly used to assess the bony structures of the jaw and can help identify fractures, tumors, or other abnormalities that may be affecting the mandibular nerve. CT scans, on the other hand, provide more detailed images and can show cross-sectional views of the jaw, allowing for a more comprehensive evaluation of the nerve and surrounding tissues.
In certain cases, an MRI scan may be ordered to further investigate the mandibular nerve. MRI scans use powerful magnets and radio waves to create detailed images of the soft tissues, including nerves. This can be particularly useful in identifying any nerve compression, inflammation, or other abnormalities that may be causing the pain.
It is important to note that while imaging tests can provide valuable information, they are not always necessary for diagnosing mandibular nerve pain. Your healthcare provider will determine the need for imaging based on your specific symptoms, medical history, and physical examination findings.
Treatment Options for Mandibular Nerve Pain
Medications for Mandibular Nerve Pain
Medication management plays a key role in treating mandibular nerve pain. Depending on the underlying cause and severity of the pain, over-the-counter pain relievers, topical creams, or prescribed medications may be recommended. It is important to consult with a healthcare professional to determine the most suitable medication regimen for your specific situation.
Non-Pharmacological Therapies
Various non-pharmacological therapies can complement medication management for mandibular nerve pain. These may include physical therapy, hot or cold compresses, acupuncture, or transcutaneous electrical nerve stimulation (TENS). These therapies can help alleviate pain, improve jaw function, and enhance overall well-being.
Surgical Interventions
In severe cases where conservative measures fail to provide relief, surgical interventions may be considered. Surgical options may include decompression procedures to alleviate nerve compression, repair or removal of damaged tissues, or corrective dental procedures. Such interventions should only be pursued under the guidance and expertise of qualified healthcare professionals.
Prevention Strategies for Mandibular Nerve Pain
Dental Hygiene and Mandibular Nerve Health
Maintaining good dental hygiene practices is crucial for promoting mandibular nerve health. Regular brushing, flossing, and dental check-ups can help prevent tooth decay and gum disease, reducing the risk of nerve-related issues.
Lifestyle Modifications to Prevent Mandibular Nerve Pain
Certain lifestyle modifications can contribute significantly to the prevention of mandibular nerve pain. These may include maintaining proper posture, avoiding excessive jaw clenching or teeth grinding, and using protective headgear during sports or other activities that pose a risk of facial injuries.
Living with Mandibular Nerve Pain
Coping Mechanisms for Chronic Pain
Living with chronic mandibular nerve pain can be challenging, both physically and emotionally. Implementing effective coping mechanisms is vital for maintaining a positive outlook and managing pain. Strategies such as relaxation techniques, mindfulness practices, and engaging in enjoyable activities can help distract from the pain and improve overall well-being.
Seeking Support for Mandibular Nerve Pain
Dealing with mandibular nerve pain can feel isolating, but it is important to remember that you are not alone. Seeking support from healthcare professionals, support groups, or online communities can provide invaluable guidance and comfort. Remember, sharing your experiences and emotions with others who can relate can make a significant difference in your journey to finding relief.
In conclusion, the complex nature of mandibular nerve pain demands a comprehensive understanding of its causes, symptoms, diagnosis, treatment, and prevention. While this article provides valuable insights into this intricate issue, it is imperative to consult with a healthcare professional for proper evaluation and personalized guidance. Together with the guidance of experts, individuals affected by mandibular nerve pain can navigate their condition with greater knowledge and confidence.