what causes mandibular nerve pain
Mandibular nerve pain, also known as trigeminal neuralgia, can be a debilitating condition that affects the quality of life for those who experience it. The mandibular nerve, which is a branch of the trigeminal nerve, provides sensation to the lower jaw, teeth, and gums. When this nerve becomes inflamed or damaged, it can result in excruciating pain that radiates throughout the face. Understanding the causes of mandibular nerve pain is crucial in order to develop effective treatment strategies for those affected.
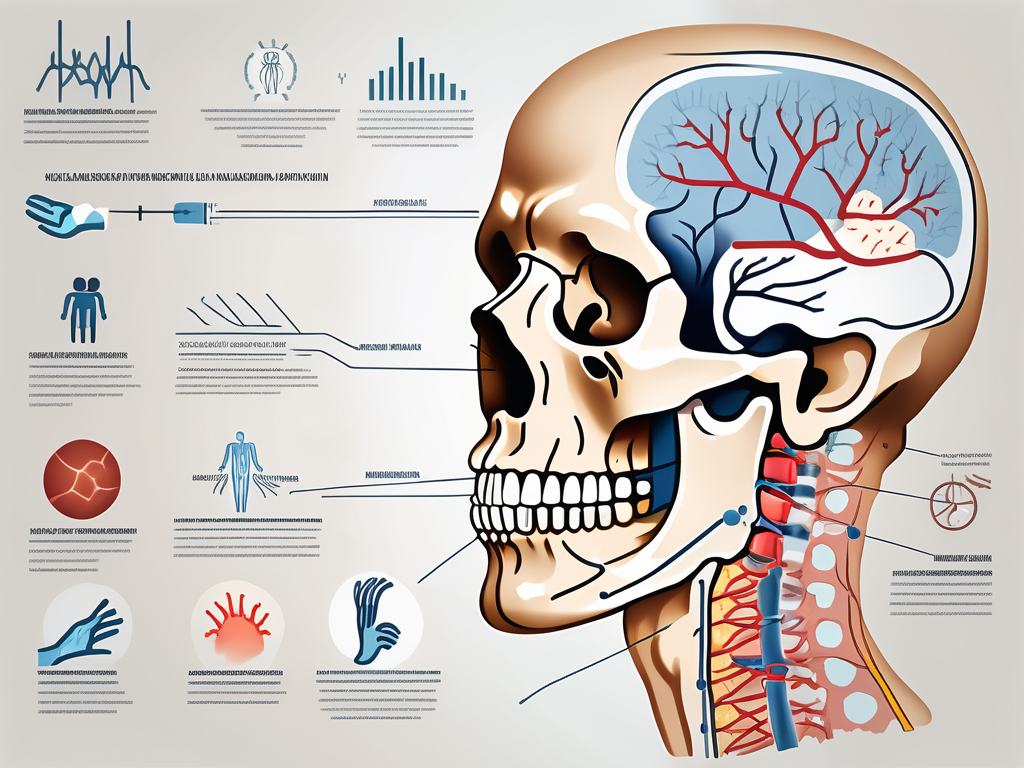
Understanding Mandibular Nerve Pain
Mandibular nerve pain is a neurological condition characterized by intermittent and severe facial pain. The mandibular nerve is responsible for transmitting sensory information from the lower jaw to the brain. When this nerve becomes irritated or compressed, it can lead to the development of pain in the affected area. It is estimated that approximately 15,000 new cases of trigeminal neuralgia are diagnosed each year in the United States alone.
Anatomy of the Mandibular Nerve
The mandibular nerve is one of the three branches of the trigeminal nerve, which is responsible for transmitting sensation from the face to the brain. This nerve passes through the skull and branches out to innervate various regions of the face, including the lower jaw, teeth, gums, and mouth. When there is damage or inflammation along the course of the mandibular nerve, it can result in the development of mandibular nerve pain.
The mandibular nerve originates from the trigeminal ganglion, a collection of nerve cell bodies located within the skull. From there, it travels through the foramen ovale, a small opening in the skull, and enters the infratemporal fossa. Within the infratemporal fossa, the mandibular nerve gives off several branches that supply sensation to different areas of the face.
One of the major branches of the mandibular nerve is the inferior alveolar nerve, which provides sensory innervation to the lower teeth and gums. This branch descends into the mandibular canal, a bony tunnel within the lower jaw, and gives off smaller branches that supply sensation to the teeth and gums on the affected side.
Common Symptoms of Mandibular Nerve Pain
The symptoms of mandibular nerve pain can vary from person to person, but they often include sudden and intense facial pain that may be triggered by routine activities such as brushing the teeth, speaking, or eating. The pain is typically described as sharp, shooting, or like an electric shock. These episodes may last for seconds to minutes and can occur in clusters throughout the day. The pain may be accompanied by muscle spasms in the jaw and can significantly impact a person’s ability to perform daily activities.
In addition to the characteristic pain, individuals with mandibular nerve pain may experience other sensory abnormalities. Some may report numbness or tingling in the affected areas, while others may have heightened sensitivity to touch or temperature changes. These sensory disturbances can further contribute to the discomfort and functional limitations experienced by individuals with mandibular nerve pain.
Furthermore, the impact of mandibular nerve pain extends beyond the physical symptoms. The unpredictable nature of the pain episodes can lead to anxiety and fear of triggering an episode, causing individuals to avoid certain activities or social situations. The chronic nature of the condition can also lead to feelings of frustration, depression, and isolation.
It is important for individuals experiencing mandibular nerve pain to seek medical evaluation and diagnosis. A thorough examination, including a detailed medical history and neurological assessment, can help determine the underlying cause of the pain and guide appropriate treatment options. Treatment may involve a combination of medications, nerve blocks, physical therapy, and in some cases, surgical interventions.
Overall, understanding the anatomy and symptoms of mandibular nerve pain is crucial in providing appropriate care and support for individuals affected by this condition. Ongoing research and advancements in the field of neurology continue to shed light on the underlying mechanisms of mandibular nerve pain, offering hope for improved management and quality of life for those living with this challenging condition.
Potential Causes of Mandibular Nerve Pain
Several factors can contribute to the development of mandibular nerve pain. Understanding these potential causes is important in order to effectively manage and treat the condition.
Dental Issues and Mandibular Nerve Pain
Dental problems, such as tooth decay, gum disease, or dental trauma, can lead to inflammation or compression of the mandibular nerve. In some cases, dental procedures or surgeries may inadvertently damage the nerve, resulting in chronic pain. It is important to maintain good oral hygiene and address any dental issues promptly to reduce the risk of developing mandibular nerve pain.
When tooth decay is left untreated, it can progress and reach the inner layers of the tooth, where the nerve is located. The bacteria that cause tooth decay release acids that can irritate and inflame the nerve, leading to pain. Regular dental check-ups and cleanings can help prevent tooth decay and minimize the risk of mandibular nerve pain.
Gum disease, also known as periodontal disease, is another potential cause of mandibular nerve pain. When plaque and tartar build up along the gumline, it can cause the gums to become infected and inflamed. This inflammation can spread to the surrounding tissues, including the mandibular nerve, causing discomfort. Proper oral hygiene, including regular brushing and flossing, as well as professional dental cleanings, can help prevent gum disease and reduce the risk of mandibular nerve pain.
In some cases, dental procedures or surgeries may inadvertently damage the mandibular nerve. This can occur during tooth extractions, root canal treatments, or dental implant placements. While these procedures are generally safe, there is a small risk of nerve injury. Dentists take precautions to minimize this risk, but it is important to be aware of the potential complications and discuss them with your dentist before undergoing any dental procedures.
Trauma and the Mandibular Nerve
Physical trauma to the face and jaw can also cause damage to the mandibular nerve, leading to the development of pain. This can occur as a result of accidents, sports injuries, or surgical procedures involving the jaw. It is essential for individuals who have experienced facial trauma to seek medical attention and undergo thorough evaluation to determine if there has been any nerve damage.
Accidents, such as falls or car collisions, can cause direct impact to the face or jaw, resulting in nerve damage. Sports injuries, especially those involving contact sports like football or boxing, can also lead to trauma to the mandibular nerve. Additionally, surgical procedures involving the jaw, such as orthognathic surgery or jaw reconstruction, carry a risk of nerve injury. It is important to follow proper safety precautions and consult with a healthcare professional to minimize the risk of mandibular nerve damage.
Infections and Mandibular Nerve Pain
Infections in the oral cavity, such as dental abscesses or herpes zoster (shingles), can cause inflammation and irritation of the mandibular nerve. This can result in persistent pain in the affected area. Proper oral hygiene and timely treatment of any oral infections are essential in reducing the risk of developing mandibular nerve pain.
A dental abscess is a pocket of pus that forms due to a bacterial infection. It can develop as a result of untreated tooth decay or gum disease. The infection can spread to the surrounding tissues, including the mandibular nerve, causing pain and discomfort. Prompt treatment, such as root canal therapy or tooth extraction, is necessary to eliminate the infection and alleviate the nerve pain.
Herpes zoster, commonly known as shingles, is a viral infection that can affect the nerves, including the mandibular nerve. It is caused by the reactivation of the varicella-zoster virus, which also causes chickenpox. Shingles typically presents as a painful rash that follows the path of the affected nerve. Antiviral medications and pain management strategies are commonly used to treat shingles and relieve the associated mandibular nerve pain.
By understanding the potential causes of mandibular nerve pain, individuals can take steps to prevent or manage the condition. Maintaining good oral hygiene, addressing dental issues promptly, and seeking medical attention for facial trauma or oral infections are all important in reducing the risk of developing mandibular nerve pain.
Diagnosing Mandibular Nerve Pain
Accurate diagnosis of mandibular nerve pain is crucial in order to develop an effective treatment plan. A thorough medical history, physical examination, and additional diagnostic tests may be necessary to determine the underlying cause of the pain.
When it comes to diagnosing mandibular nerve pain, healthcare providers employ a comprehensive approach. They start by taking a detailed medical history, delving into the nature and characteristics of the pain. They inquire about any triggering factors or associated symptoms that may provide valuable clues about the underlying cause.
During the physical examination, healthcare providers focus on the head, face, and oral cavity. They carefully assess for any signs of inflammation, trauma, or infection that may be contributing to the pain. By examining the affected area, they can gather important information about the condition of the mandibular nerve and its surrounding structures.
Medical History and Physical Examination
During the initial evaluation, the healthcare provider will inquire about the nature and characteristics of the pain, as well as any triggering factors or associated symptoms. A comprehensive physical examination, focusing on the head, face, and oral cavity, will be performed to assess for any signs of inflammation, trauma, or infection.
Moreover, healthcare providers also pay attention to the patient’s overall health and medical history. They explore any pre-existing medical conditions or previous injuries that may be relevant to the current pain. This comprehensive approach helps healthcare providers gain a holistic understanding of the patient’s condition and aids in accurate diagnosis.
Imaging Techniques for Detecting Mandibular Nerve Issues
In some cases, imaging studies such as X-rays, magnetic resonance imaging (MRI), or computed tomography (CT) scans may be ordered to visualize the mandibular nerve and surrounding structures. These imaging techniques can provide valuable information regarding any structural abnormalities or nerve compression that may be contributing to the pain.
X-rays are commonly used to assess the bony structures of the jaw and detect any fractures or abnormalities. They provide a detailed view of the mandible, allowing healthcare providers to identify any potential issues that may be affecting the mandibular nerve.
MRI scans utilize powerful magnets and radio waves to create detailed images of the soft tissues in the jaw. This imaging technique is particularly useful in identifying nerve-related problems, such as inflammation, compression, or tumors. By visualizing the mandibular nerve and its surrounding structures, healthcare providers can pinpoint the exact source of the pain.
CT scans, on the other hand, provide cross-sectional images of the jaw and can reveal any structural abnormalities or changes in the bone density. This imaging technique is especially helpful in detecting fractures, infections, or other conditions that may be causing mandibular nerve pain.
By utilizing these advanced imaging techniques, healthcare providers can gain a deeper understanding of the mandibular nerve and its surrounding structures. This knowledge is crucial in accurately diagnosing the underlying cause of the pain and developing an effective treatment plan.
Treatment Options for Mandibular Nerve Pain
The management of mandibular nerve pain typically involves a multidisciplinary approach, tailored to the individual patient’s needs and the underlying cause of the pain. This comprehensive approach ensures that all aspects of the condition are addressed, leading to better outcomes and improved quality of life.
When it comes to treating mandibular nerve pain, there are several options available, ranging from medications to surgical interventions and alternative therapies. The choice of treatment depends on various factors, including the severity of the pain, the underlying cause, and the patient’s overall health.
Medications for Mandibular Nerve Pain
The first line of treatment for mandibular nerve pain often involves medications aimed at alleviating pain and reducing nerve inflammation. Anticonvulsant medications, such as carbamazepine or gabapentin, are commonly prescribed to help control the episodes of pain. These medications work by stabilizing the overactive nerves, reducing their sensitivity, and preventing the transmission of pain signals. Additionally, antidepressant medications, such as amitriptyline, may be utilized to modulate pain signals in the central nervous system, providing relief from the debilitating symptoms of mandibular nerve pain.
It is important to consult with a healthcare professional before starting any medication and to follow their guidance closely. They will consider factors such as potential side effects, drug interactions, and individual patient characteristics to determine the most appropriate medication and dosage.
Surgical Interventions for Mandibular Nerve Pain
In cases where conservative measures fail to provide relief, surgical interventions may be considered. These procedures aim at decompressing or ablating the affected nerve to alleviate the pain. Microvascular decompression is a surgical technique that involves repositioning blood vessels that may be compressing the nerve, thereby relieving the pressure and reducing pain. Another option is radiofrequency ablation, which uses heat to destroy the nerve fibers responsible for transmitting pain signals. Nerve blocks, where medication is injected into or around the affected nerve, can also provide temporary relief from mandibular nerve pain.
It is important to note that these procedures are generally performed by specialists who have expertise in treating nerve-related pain. A thorough evaluation is necessary to determine the appropriateness of the intervention, taking into consideration the patient’s overall health, the severity of the pain, and the potential risks and benefits of the procedure.
Alternative Therapies for Mandibular Nerve Pain
In addition to traditional medical treatments, alternative therapies such as acupuncture, transcutaneous electrical nerve stimulation (TENS), or biofeedback may be utilized in the management of mandibular nerve pain. These therapies aim to stimulate the body’s natural healing mechanisms and promote pain relief. Acupuncture involves the insertion of thin needles into specific points on the body, which can help restore the balance of energy and reduce pain. TENS therapy uses low-voltage electrical currents to stimulate the nerves and disrupt the transmission of pain signals. Biofeedback, on the other hand, involves the use of electronic devices to monitor and control bodily functions, such as muscle tension and heart rate, helping individuals gain control over their pain response.
While there is limited scientific evidence to support their efficacy, some individuals may find these complementary approaches helpful in reducing pain and improving overall well-being. It is important to discuss these options with a healthcare provider to ensure they are safe and appropriate for individual use. They can provide guidance on the potential benefits and risks of these alternative therapies and help determine the best course of action.
Prevention of Mandibular Nerve Pain
While not all cases of mandibular nerve pain can be prevented, there are steps individuals can take to reduce the risk of developing this condition.
Regular Dental Check-ups
Maintaining good oral hygiene and scheduling routine dental check-ups are essential in preventing dental issues that may lead to mandibular nerve pain. Regular dental cleanings, X-rays, and prompt treatment of dental problems can help identify and address any issues before they escalate into more significant complications.
Protective Measures for the Jaw
Individuals involved in contact sports or activities with a high risk of facial trauma should wear appropriate protective gear, such as mouthguards or helmets. Taking preventive measures to protect the jaw can significantly reduce the risk of injury to the mandibular nerve.
Healthy Lifestyle Choices to Prevent Mandibular Nerve Pain
Adopting a healthy lifestyle, including a balanced diet, regular exercise, stress management, and adequate sleep, can contribute to overall well-being and potentially reduce the risk of developing chronic pain conditions. It is important to prioritize self-care and maintain a healthy lifestyle to support overall health.
In conclusion, mandibular nerve pain can have a profound impact on an individual’s quality of life. Understanding the causes and potential risk factors associated with this condition is crucial in order to develop appropriate strategies for prevention, diagnosis, and management. It is essential for individuals experiencing symptoms of mandibular nerve pain to seek medical attention and consult with healthcare professionals who specialize in the diagnosis and treatment of facial pain. With appropriate care, support, and management, individuals affected by mandibular nerve pain can find relief and regain control of their lives.