if there is damage to the mandibular nerve during oral surgery, what are the symtpoms of this
If there is damage to the mandibular nerve during oral surgery, it is important to be aware of the potential symptoms that may arise. The mandibular nerve is a significant branch of the trigeminal nerve, which is responsible for providing sensory and motor innervation to the lower part of the face, including the jaw, lower teeth, and surrounding tissues. In this article, we will explore the anatomy of the mandibular nerve, discuss the potential causes of nerve damage during oral surgery, identify the symptoms that may indicate nerve damage, discuss diagnostic procedures, outline treatment options, and suggest preventative measures. It is worth noting that the information presented here should not be taken as medical advice, and if you experience any of the symptoms discussed, it is crucial to consult with a qualified healthcare professional promptly.
Understanding the Mandibular Nerve
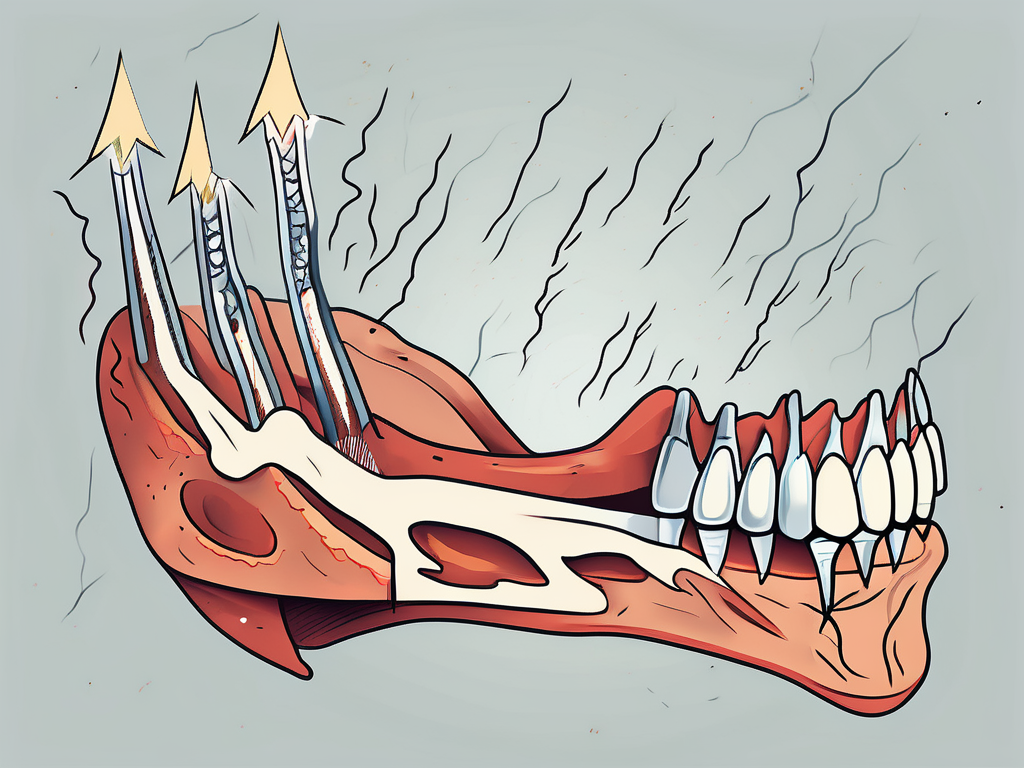
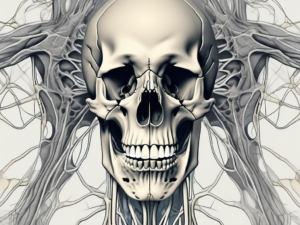
The mandibular nerve, also known as the V3 branch of the trigeminal nerve, is a crucial component of the cranial nerves. It is the largest branch of the trigeminal nerve and arises from the sensory nucleus of the trigeminal nerve within the brainstem. This nerve extends through the skull and passes through the mandibular foramen, a small opening in the mandible bone, to supply sensation to the lower jaw.
As its name suggests, the mandibular nerve not only provides sensory innervation but also controls the muscles responsible for chewing. This makes it an essential player in the complex process of mastication, allowing us to break down food into smaller, more digestible pieces.
Anatomy of the Mandibular Nerve
The mandibular nerve consists of several branches, each serving a specific region. These branches include the auriculotemporal nerve, inferior alveolar nerve, mental nerve, and lingual nerve.
The auriculotemporal nerve, one of the branches of the mandibular nerve, provides sensory innervation to the temple region and the side of the head. It plays a role in transmitting pain, temperature, and touch sensations from these areas.
The inferior alveolar nerve, another branch of the mandibular nerve, supplies sensation to the lower teeth and gums. It is responsible for transmitting sensory information, allowing us to perceive sensations such as pressure, temperature, and pain in the lower dental arch.
The mental nerve, yet another branch of the mandibular nerve, provides sensation to the chin and lower lip. It allows us to perceive touch, temperature, and pain in these areas, contributing to our overall sensory experience.
The lingual nerve, the final branch of the mandibular nerve, supplies sensation to the tongue. It plays a crucial role in our ability to taste, perceive temperature, and experience touch on the surface of the tongue.
Role of the Mandibular Nerve in Oral Functioning
The mandibular nerve plays a vital role in various aspects of oral functioning. Its involvement in chewing, biting, speech, and sensation highlights its significance in our daily lives.
When we chew, the mandibular nerve coordinates the movement of the muscles responsible for mastication. It ensures that our jaw moves in a synchronized manner, allowing us to break down food into smaller particles, making digestion easier.
In addition to chewing, the mandibular nerve also contributes to our ability to bite. It provides the necessary sensory feedback, allowing us to gauge the force required for biting into different foods and objects.
Speech is another area where the mandibular nerve plays a role. It helps control the muscles involved in articulation, allowing us to produce clear and intelligible speech sounds.
Furthermore, the mandibular nerve is responsible for providing sensation to the lower jaw, teeth, gums, chin, lower lip, and tongue. This sensory feedback allows us to perceive various stimuli, such as pain, temperature, and touch, ensuring that we can respond appropriately to our environment.
Given the crucial role of the mandibular nerve in oral functioning, any damage or impairment to this nerve can lead to significant impairments in chewing, biting, speech, and sensation. These impairments can have a profound impact on a person’s quality of life, affecting their ability to eat, communicate, and experience the world around them.
Potential Causes of Mandibular Nerve Damage
Mandibular nerve damage can occur due to various factors, including risks associated with oral surgery and other factors that contribute to nerve damage.
The mandibular nerve, also known as the inferior alveolar nerve, is a branch of the trigeminal nerve that provides sensation to the lower teeth, gums, and lower lip. Damage to this nerve can result in numbness, tingling, or pain in these areas.
Risks Associated with Oral Surgery
Oral surgery procedures, such as wisdom tooth extraction, dental implant placement, or corrective jaw surgery, carry inherent risks, including the possibility of mandibular nerve damage. Factors that increase the risk of nerve injury during these procedures include the proximity of the nerve to the surgical site, the complexity of the surgery, and the surgeon’s skill and expertise.
During wisdom tooth extraction, for example, the roots of the tooth may be located close to the mandibular nerve. If the surgeon is not careful, they may inadvertently damage the nerve while removing the tooth. Similarly, during dental implant placement, the implant may need to be inserted near the nerve, increasing the risk of injury.
Furthermore, corrective jaw surgery, which involves repositioning the jaw to correct bite abnormalities, can also pose a risk to the mandibular nerve. The nerve may be stretched or compressed during the surgical procedure, leading to temporary or permanent damage.
Other Factors Contributing to Nerve Damage
In addition to surgical risks, certain systemic conditions, such as diabetes or autoimmune diseases, can increase the likelihood of nerve damage during oral surgery. These conditions can affect nerve function and impair the body’s ability to heal, making the nerves more susceptible to injury.
Trauma to the face or jaw can also contribute to mandibular nerve damage. Accidents, falls, or sports injuries that involve a direct blow to the face can result in nerve injury. The force of impact can cause the nerve to be compressed, stretched, or even severed.
Infections in the oral cavity, such as abscesses or cellulitis, can also lead to nerve damage. The inflammation and swelling associated with these infections can put pressure on the nerve, causing pain and dysfunction.
Additionally, the presence of a tumor in the vicinity of the mandibular nerve can pose a risk. Tumors can exert pressure on the nerve, leading to symptoms such as numbness or tingling in the affected area.
It is important for individuals undergoing oral surgery or experiencing symptoms of mandibular nerve damage to consult with a qualified healthcare professional. Early diagnosis and appropriate treatment can help prevent further complications and promote recovery.
Identifying Symptoms of Mandibular Nerve Damage
Mandibular nerve damage can manifest in various ways, and recognizing the symptoms is crucial for timely diagnosis and appropriate management.
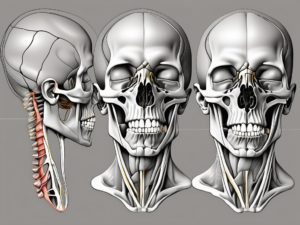
When it comes to physical symptoms of mandibular nerve damage, there are several key indicators to be aware of. One common manifestation is weakness or paralysis of the muscles responsible for chewing. This can make it difficult to open or close the mouth properly, resulting in reduced bite force and potentially asymmetrical movement of the jaw. It’s important to note that these physical symptoms can vary in severity from person to person.
In addition to muscle weakness, mandibular nerve damage can also lead to an altered appearance. For example, some individuals may experience a drooping lower lip or sagging of the lower face on one side. These changes in facial structure can be distressing and may impact a person’s self-esteem and overall well-being.
Turning our attention to sensory symptoms, it’s not uncommon for individuals with mandibular nerve damage to experience numbness or tingling in the lower lip, chin, gums, or tongue. This altered or loss of sensation can have a significant impact on daily activities such as eating, drinking, and speaking. It’s important to be mindful of these sensory changes to avoid accidental biting or burning of the affected area.
Speech and eating difficulties can also arise as a result of mandibular nerve damage. Dysarthria, a condition characterized by difficulty articulating speech, may occur. This can make it challenging to communicate effectively, impacting both personal and professional interactions. Furthermore, the ability to chew food adequately and speak clearly can be compromised, leading to frustration and potential social isolation.
It’s worth noting that the symptoms mentioned above are not an exhaustive list, and individuals may experience additional or different symptoms depending on the extent and location of the nerve damage. If you suspect you may have mandibular nerve damage, it is important to consult with a healthcare professional for a comprehensive evaluation and appropriate management.
Diagnostic Procedures for Mandibular Nerve Damage
To confirm the presence of mandibular nerve damage and determine its extent, various diagnostic procedures are available. These procedures provide valuable information to healthcare professionals, enabling them to accurately diagnose and effectively treat patients with mandibular nerve damage.
Clinical Examination
A comprehensive clinical examination is typically the first step in diagnosing mandibular nerve damage. During this examination, the healthcare professional carefully evaluates the patient’s symptoms and medical history. They may also perform a physical examination of the affected area, assessing muscle strength and tone, evaluating sensation in the affected areas, and examining the patient’s ability to perform specific tasks, such as biting and chewing. Through this thorough assessment, the healthcare professional can gather important clues about the nature and severity of the nerve damage.
Furthermore, the clinical examination may involve additional tests, such as assessing the patient’s reflexes and conducting sensory examinations. These tests help to identify any abnormalities or deficits in nerve function, providing further insights into the extent of the mandibular nerve damage.
Imaging Techniques
In addition to the clinical examination, imaging techniques play a crucial role in the diagnosis of mandibular nerve damage. These techniques allow healthcare professionals to visualize the bony structures surrounding the nerve and identify any abnormalities or lesions contributing to the nerve damage.
X-rays, a commonly used imaging technique, provide a detailed view of the mandible and can help identify fractures or other structural abnormalities that may be affecting the mandibular nerve. Computed tomography (CT) scans, on the other hand, provide cross-sectional images of the mandible and surrounding structures, offering a more comprehensive assessment of the nerve and any potential damage. Magnetic resonance imaging (MRI) is another powerful imaging tool that uses magnetic fields and radio waves to generate detailed images of the mandibular nerve and surrounding tissues. MRI is particularly useful in identifying soft tissue abnormalities and can provide valuable information about the extent and location of the nerve damage.
Neurological Tests
Neurological tests are another important component of the diagnostic process for mandibular nerve damage. These tests help assess the functionality of the nerve and identify the extent of damage.
Electromyography (EMG) is a commonly used neurological test that measures the electrical activity generated by the muscles innervated by the mandibular nerve. By inserting small, fine needles into the muscles, the healthcare professional can evaluate the muscle’s response to electrical stimulation. This test can help identify any abnormalities in muscle function and determine if the mandibular nerve is transmitting signals properly.
Nerve conduction studies are another type of neurological test that can be used to assess the functionality of the mandibular nerve. During this test, small electrodes are placed on the skin overlying the nerve, and a small electrical impulse is applied. By measuring the speed at which the nerve impulses travel, healthcare professionals can determine if there are any disruptions or delays in the nerve’s function.
These diagnostic procedures, including the clinical examination, imaging techniques, and neurological tests, work together to provide a comprehensive evaluation of mandibular nerve damage. By utilizing these tools, healthcare professionals can accurately diagnose the condition and develop an appropriate treatment plan tailored to each patient’s specific needs.
Treatment Options for Mandibular Nerve Damage
The approach to treating mandibular nerve damage depends on various factors, including the cause and severity of the injury.
Mandibular nerve damage can occur due to various reasons such as trauma, infection, or underlying medical conditions. It can result in a range of symptoms including pain, numbness, tingling, and difficulty in chewing or speaking.
Non-Surgical Interventions
In mild cases of mandibular nerve damage, non-surgical interventions may be recommended. These can include physical therapy exercises, pain management techniques, and lifestyle modifications to accommodate any functional limitations.
Physical therapy exercises for mandibular nerve damage focus on strengthening the muscles around the jaw and improving range of motion. These exercises can help in reducing pain, improving chewing ability, and restoring normal jaw function.
Pain management techniques may involve the use of medications such as nonsteroidal anti-inflammatory drugs (NSAIDs) or nerve pain medications to alleviate discomfort and improve quality of life. Additionally, lifestyle modifications such as avoiding hard or chewy foods and practicing stress-reducing techniques can also be beneficial.
Surgical Remedies
In more severe cases, surgical intervention may be necessary to repair or restore the damaged nerve. Different surgical approaches exist, such as nerve grafting, nerve transfer, or microsurgery techniques, wherein damaged nerve sections are repaired or replaced with healthy nerve tissue.
Nerve grafting involves taking a healthy nerve from another part of the body, such as the leg, and using it to bridge the gap in the damaged mandibular nerve. This procedure allows for the regeneration of nerve fibers and restoration of function.
Nerve transfer involves transferring a nearby healthy nerve to the damaged mandibular nerve. This technique can help restore sensation and motor function to the affected area.
Microsurgery techniques involve using specialized instruments and a high-powered microscope to repair or reconnect damaged nerve fibers. This precise approach allows for optimal nerve regeneration and functional recovery.
Rehabilitation and Recovery
Following surgical intervention, a period of rehabilitation is often required. This may involve a combination of physical therapy, speech therapy, and occupational therapy to enhance motor function, sensory perception, and overall quality of life.
Physical therapy focuses on improving jaw mobility, strength, and coordination. It may include exercises to stretch and strengthen the muscles around the jaw, as well as techniques to improve chewing and swallowing abilities.
Speech therapy can help individuals with mandibular nerve damage regain proper speech and articulation. Therapists may work on exercises to improve tongue and lip control, as well as strategies to compensate for any speech difficulties.
Occupational therapy aims to assist individuals in adapting to any functional limitations resulting from mandibular nerve damage. This may involve techniques to improve fine motor skills, such as writing or eating, and recommendations for assistive devices if needed.
Recovery from mandibular nerve damage can vary depending on the individual and the extent of the injury. It may take several months or longer to achieve optimal functional outcomes. Regular follow-up appointments with healthcare professionals are important to monitor progress and make any necessary adjustments to the treatment plan.
Prevention of Mandibular Nerve Damage
Preventing mandibular nerve damage is of paramount importance. By implementing appropriate precautions, the risk of nerve injury during oral surgery can be significantly reduced.
Pre-Surgery Precautions
Prior to oral surgery, a thorough assessment of the patient’s medical history, including any pre-existing conditions or medications, helps identify potential risk factors for nerve damage. This allows the surgeon to customize the treatment plan accordingly and minimize the chances of nerve injury.
Intraoperative Techniques
During surgery, utilizing modern technologies, such as cone-beam computed tomography (CBCT) imaging or intraoperative nerve monitoring, can aid in visualizing the nerve and avoiding accidental damage.
Post-Surgery Care Measures
Following oral surgery, complying with post-operative instructions, including taking prescribed medications, maintaining proper oral hygiene, and attending all follow-up appointments, is crucial for optimal healing and reducing the risk of complications.
In conclusion, if damage to the mandibular nerve occurs during oral surgery, it can lead to a range of symptoms affecting both physical and sensory aspects of oral functioning. Identifying these symptoms early and seeking prompt medical attention is essential for accurate diagnosis and appropriate management. While surgical and non-surgical treatment options exist, prevention remains the most effective approach. By implementing pre-surgery precautions, utilizing intraoperative techniques, and following post-surgery care measures, the risk of mandibular nerve damage can be significantly minimized. If you experience any symptoms indicative of mandibular nerve damage, consult with a qualified healthcare professional for a comprehensive evaluation and personalized care plan.