mandibular nerve innervates which muscles
The mandibular nerve is a crucial component of the trigeminal nerve, which is responsible for the sensation and motor function of the face. One of the key functions of the mandibular nerve is to innervate several important muscles involved in chewing and other movements of the jaw. Understanding the anatomy and functions of the mandibular nerve is essential for comprehending its role in muscle movement, as well as recognizing the disorders associated with this nerve.
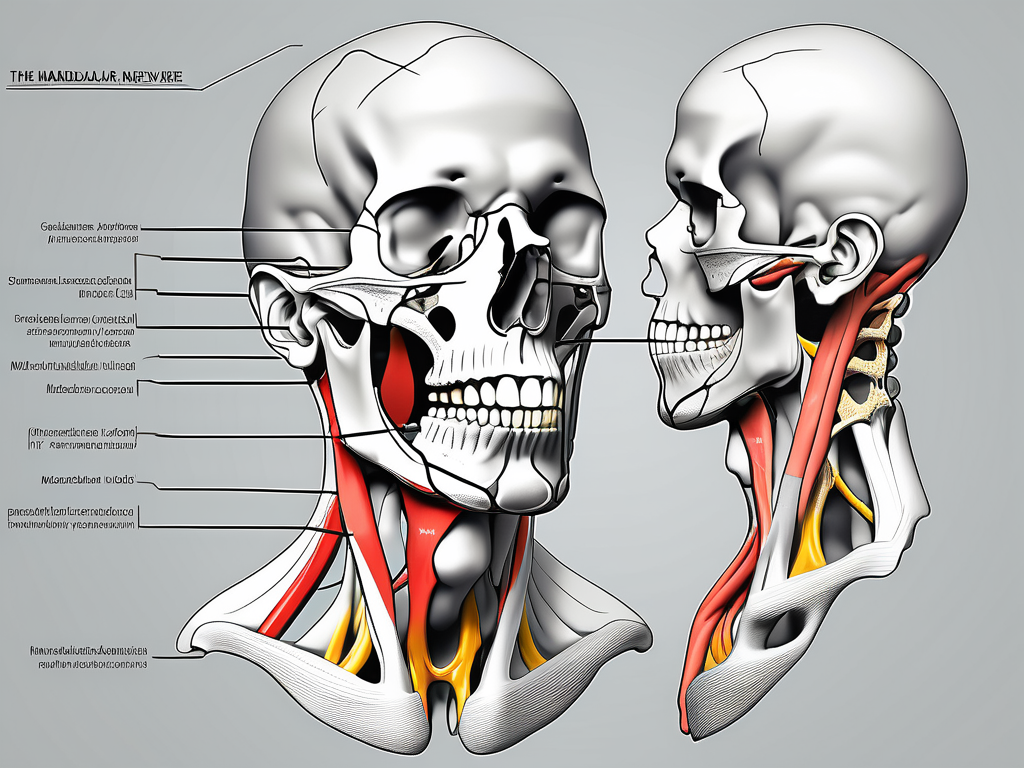
Understanding the Mandibular Nerve
The mandibular nerve, also known as the V3 branch of the trigeminal nerve, is the largest of the three divisions. It emerges from the skull through the foramen ovale and innervates various muscles of mastication, as well as other structures in the region.
The mandibular nerve is a complex network of sensory and motor fibers that provide innervation to different areas of the face. It plays a crucial role in the functioning of the lower face and jaw, allowing for movements such as biting, chewing, and speaking.
Anatomy of the Mandibular Nerve
The mandibular nerve originates from the trigeminal ganglion, which is located within the middle cranial fossa. This ganglion is a collection of nerve cell bodies that serve as a relay station for sensory information. From the trigeminal ganglion, the mandibular nerve branches out and extends towards the lower face and jaw.
Within the mandibular nerve, there are both sensory and motor fibers. The sensory fibers transmit information from the skin, teeth, and mucous membranes of the lower face and jaw. These fibers allow us to perceive sensations such as touch, temperature, and pain in this region. On the other hand, the motor fibers control the movement of specific muscles involved in mastication, such as the temporalis, masseter, and pterygoid muscles.
Functions of the Mandibular Nerve
The mandibular nerve serves several important functions in addition to its role in muscle innervation. One of its primary functions is to provide sensory feedback from the lower face. It conveys sensations such as touch, temperature, and pain from the skin, teeth, and gums of the mandible. This sensory information is crucial for our ability to perceive and respond to stimuli in the surrounding environment.
Furthermore, the mandibular nerve plays a critical role in controlling reflexes, such as the biting and chewing reflexes. These reflexes are essential for the proper functioning of the jaw and allow us to break down food into smaller, more manageable pieces for digestion.
Additionally, the mandibular nerve is involved in the regulation of salivary glands. It carries parasympathetic fibers that stimulate the production and secretion of saliva, which is essential for the lubrication and digestion of food.
In summary, the mandibular nerve is a complex and vital component of the trigeminal nerve. It provides both sensory and motor innervation to the lower face and jaw, allowing for various functions such as mastication, sensation, and reflexes. Understanding the anatomy and functions of the mandibular nerve is crucial for healthcare professionals in diagnosing and treating conditions that may affect its normal functioning.
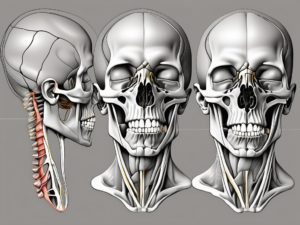
The Muscles Innervated by the Mandibular Nerve
The mandibular nerve, a branch of the trigeminal nerve, is responsible for innervating several important muscles involved in the movement of the jaw. These muscles, which play a fundamental role in chewing and speaking, include the masseter muscle, temporalis muscle, and medial and lateral pterygoid muscles.
Masseter Muscle and the Mandibular Nerve
The masseter muscle, often referred to as the “chewing muscle,” is a powerful muscle located in the jaw region. It is responsible for closing the jaw during chewing and biting. This muscle receives motor innervation from the mandibular nerve, specifically from its masseteric branch. The mandibular nerve’s innervation allows the masseter muscle to contract and exert the necessary force for effective mastication. Additionally, the masseter muscle contributes to the shape and contour of the face, providing definition to the lower jawline.
Temporalis Muscle and the Mandibular Nerve
The temporalis muscle is a fan-shaped muscle that covers the temporal region of the skull. It plays a crucial role in the process of chewing by elevating and retracting the mandible. The mandibular nerve provides motor innervation to the temporalis muscle through its deep temporal branches. This innervation allows the temporalis muscle to contract and exert the necessary force for biting and grinding food. In addition to its role in mastication, the temporalis muscle also contributes to facial expressions, such as clenching the jaw in moments of concentration or stress.
Medial and Lateral Pterygoid Muscles and the Mandibular Nerve
The medial and lateral pterygoid muscles are located in the deep regions of the face, specifically within the pterygopalatine fossa and infratemporal fossa. These muscles are involved in several complex movements of the jaw, including side-to-side and forward-backward movements. The mandibular nerve provides motor innervation to both the medial and lateral pterygoid muscles through its branches, such as the nerve to the medial pterygoid and nerve to the lateral pterygoid. This innervation enables the pterygoid muscles to coordinate their actions, allowing for precise control over the movements of the mandible during chewing, speaking, and swallowing.
In summary, the mandibular nerve plays a vital role in innervating the muscles responsible for the movement and function of the jaw. The masseter muscle, temporalis muscle, and medial and lateral pterygoid muscles all rely on the motor innervation provided by the mandibular nerve to carry out their respective functions in the complex process of mastication. Understanding the innervation of these muscles is crucial for dental professionals, oral surgeons, and researchers studying the mechanics of the jaw.
The Role of the Mandibular Nerve in Muscle Movement
The mandibular nerve plays a crucial role in the movement and coordination of the muscles involved in chewing and other activities related to the jaw. By supplying motor innervation to these muscles, the mandibular nerve ensures the precise and synchronized contractions required for efficient mastication and articulation.
In addition to its role in chewing, the mandibular nerve also has an impact on various other functions related to the jaw and facial muscles. It plays a significant role in facial expressions, allowing for the movement and control of the muscles involved in smiling, frowning, and other facial gestures. The precise coordination provided by the mandibular nerve ensures that these expressions are accurately conveyed.
How the Mandibular Nerve Affects Chewing
During the process of chewing, the mandibular nerve coordinates the movements of the muscles involved, allowing for the efficient breakdown of food. This coordination is essential to ensure that the jaw muscles work in harmony, exerting the appropriate amount of force to grind and crush food into smaller, more manageable pieces.
Furthermore, the mandibular nerve also plays a role in regulating the speed and rhythm of chewing. It ensures that the jaw muscles contract and relax in a coordinated manner, allowing for the smooth and efficient movement of the lower jaw. This coordination is crucial for preventing any discomfort or strain during the chewing process.
Any disruption or dysfunction of the mandibular nerve can lead to difficulties in chewing, resulting in complications like inadequate mastication and poor digestion. It can also lead to pain and discomfort in the jaw, making it challenging to enjoy meals and maintain proper nutrition.
The Impact of the Mandibular Nerve on Speech
Besides aiding in chewing, the mandibular nerve also contributes to the production of clear and intelligible speech. The precise control it provides over the movements of the jaw muscles ensures proper articulation of words and enhances the clarity of speech.
When we speak, the mandibular nerve works in conjunction with other cranial nerves to coordinate the movements of the tongue, lips, and vocal cords. This coordination allows for the precise production of different sounds and facilitates effective communication.
Any impairment of the mandibular nerve can potentially affect speech production and clarity. It may result in difficulties pronouncing certain sounds or words, leading to speech impediments or reduced intelligibility. Speech therapy and other interventions may be necessary to help individuals overcome these challenges and improve their communication abilities.
Disorders Related to the Mandibular Nerve
While the mandibular nerve is a vital component of facial function, it is susceptible to various disorders that can impair its proper functioning and cause significant discomfort.
The mandibular nerve, also known as the inferior alveolar nerve, is a branch of the trigeminal nerve. It provides sensory innervation to the lower teeth, gums, and lower lip, as well as motor innervation to the muscles responsible for chewing. Any disruption or damage to this nerve can lead to a range of disorders and symptoms.
Trigeminal Neuralgia and the Mandibular Nerve
One of the most notable disorders associated with the mandibular nerve is trigeminal neuralgia. This condition is characterized by intense facial pain, typically caused by irritation or compression of the trigeminal nerve branches, including the mandibular nerve.
The pain experienced in trigeminal neuralgia is often described as sharp, shooting, or electric shock-like. It can be triggered by simple activities such as talking, eating, or even touching the face. The pain episodes can be brief but excruciating, leading to significant distress and impairment in daily life.
Trigeminal neuralgia can be caused by various factors, including blood vessel compression, nerve damage, or underlying medical conditions such as multiple sclerosis. Treatment options for trigeminal neuralgia may include medication, nerve blocks, or surgical interventions, depending on the severity and underlying cause of the condition.
If you experience unexplained facial pain or other symptoms suggestive of trigeminal neuralgia, it is crucial to consult with a healthcare professional for an accurate diagnosis and appropriate treatment options.
Mandibular Nerve Neuropathy
Mandibular nerve neuropathy, also known as mandibular nerve dysfunction or damage, can occur due to various factors such as trauma, infections, or underlying medical conditions.
When the mandibular nerve is affected, it can result in a range of symptoms, including facial weakness, numbness, or pain. Patients may experience difficulty in opening or closing their mouths, chewing food, or even speaking clearly. The severity of symptoms can vary depending on the extent and location of the nerve damage.
Diagnosing mandibular nerve neuropathy involves a thorough medical history, physical examination, and sometimes additional tests such as imaging studies or nerve conduction studies. Treatment options for mandibular nerve neuropathy depend on the underlying cause and may include medications, physical therapy, or in some cases, surgical interventions.
If you suspect you may have mandibular nerve neuropathy, seeking medical advice is essential to determine the underlying cause and manage the condition effectively.
Treatment and Management of Mandibular Nerve Disorders
When dealing with disorders of the mandibular nerve, appropriate treatment and management strategies are crucial for symptomatic relief and improved quality of life.
The mandibular nerve, also known as the inferior alveolar nerve, is a branch of the trigeminal nerve that innervates the lower teeth, lower lip, and chin. It plays a vital role in sensation and motor function of the lower face, making any dysfunction in this nerve a significant concern.
Medical Interventions for Mandibular Nerve Disorders
The treatment of mandibular nerve disorders often involves a multimodal approach. This may include medication to alleviate pain, reduce inflammation, or manage any underlying conditions contributing to nerve dysfunction. Nonsteroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen or corticosteroids may be prescribed to reduce inflammation and provide pain relief. Anticonvulsant medications like gabapentin or pregabalin may also be used to manage neuropathic pain associated with mandibular nerve disorders.
Consultation with a healthcare professional is essential to determine the most appropriate medical interventions based on the individual’s specific condition. In some cases, referral to a neurologist or pain management specialist may be necessary to optimize treatment outcomes.
Surgical Options for Mandibular Nerve Disorders
In more severe cases, surgical interventions may be required to address certain mandibular nerve disorders. Surgical procedures vary depending on the specific condition and its underlying cause. These procedures may involve decompression of the nerve, removal of a tumor or lesion compressing the nerve, or other targeted interventions designed to alleviate symptoms and restore normal nerve function.
Microvascular decompression is a surgical technique that involves relieving pressure on the mandibular nerve by placing a cushioning material between the nerve and the compressing structure. This procedure can be highly effective in providing long-term relief for individuals with nerve compression.
Rehabilitation and Therapy for Mandibular Nerve Disorders
In addition to medical and surgical interventions, rehabilitation and therapy play an essential role in the management of mandibular nerve disorders. Physical therapy can help restore muscle strength and coordination, while speech therapy may be beneficial for individuals experiencing speech difficulties.
Physical therapy for mandibular nerve disorders typically involves exercises to improve jaw mobility and strengthen the muscles involved in chewing. This may include techniques such as jaw stretching, resistance training, and coordination exercises. Speech therapy focuses on improving articulation and clarity of speech through targeted exercises and techniques.
A comprehensive rehabilitation and therapy plan, developed in collaboration with healthcare professionals, can significantly improve functional outcomes for individuals with mandibular nerve disorders. This may include a combination of in-person sessions and at-home exercises to ensure consistent progress and optimal recovery.
In conclusion, the mandibular nerve innervates crucial muscles involved in chewing and other movements of the jaw. Understanding its anatomy, functions, and role in muscle movement is essential in comprehending the complex nature of its disorders. If you suspect any issues related to the mandibular nerve, it is important to seek medical advice promptly to determine the most appropriate diagnosis and therapeutic interventions. The intricate connection between the mandibular nerve and its associated muscles highlights the importance of maintaining optimal neural function for efficient mastication, proper speech articulation, and overall facial functioning.