what is the mandibular nerve called anterior to the mental foramen
The mandibular nerve, also known as the inferior alveolar nerve, undergoes a name change as it passes anterior to the mental foramen. This article aims to provide a comprehensive understanding of the anatomy, function, and clinical significance of the mandibular nerve in relation to the mental foramen.
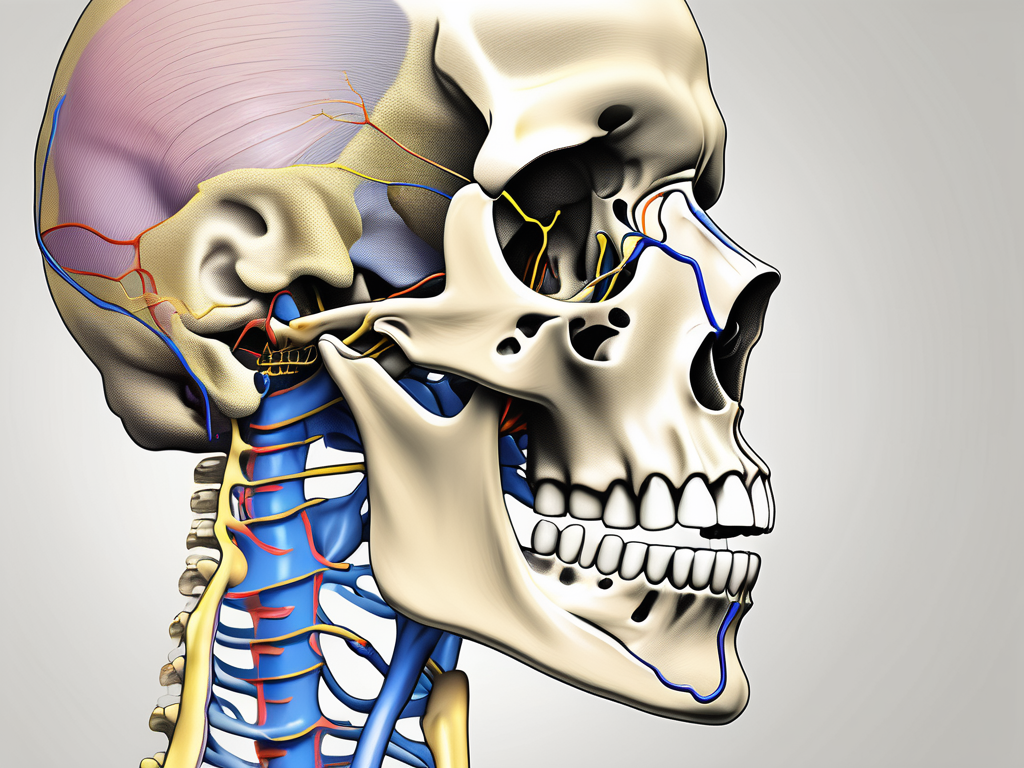
Understanding the Anatomy of the Mandibular Nerve
The mandibular nerve is one of the three main branches of the trigeminal nerve, the largest cranial nerve. It is responsible for providing sensory innervation to the lower teeth, gums, lower lip, chin, and the floor of the mouth. It also plays a crucial role in motor functions, controlling the muscles involved in chewing.
The mandibular nerve, also known as the V3 branch of the trigeminal nerve, is a complex structure with a fascinating anatomy. Let’s delve deeper into the intricacies of this nerve and explore its role in facial sensation.
The Role of the Mandibular Nerve in Facial Sensation
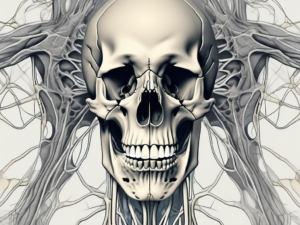
The mandibular nerve carries sensory information from various regions of the face. It contains sensory fibers that transmit touch, temperature, and pain signals from the lower face to the brain. This enables us to perceive sensations and respond accordingly.
When you bite into a juicy apple, the mandibular nerve is responsible for relaying the sensation of the crisp texture and sweet taste to your brain. It also alerts you to any potential dangers, such as a sharp object hidden within the fruit.
Moreover, the mandibular nerve plays a vital role in maintaining the integrity of our oral cavity. It allows us to sense the temperature of our food, ensuring we don’t burn our tongues on a scalding hot beverage or freeze our teeth with an icy treat.
The Pathway of the Mandibular Nerve
The mandibular nerve originates from the trigeminal ganglion within the skull. It passes through the foramen ovale, a bony opening in the skull, and continues its course within the infratemporal fossa. As it approaches the mandible, the nerve gives off branches that supply different structures, such as the auriculotemporal nerve and the lingual nerve.
Imagine the mandibular nerve as a highway, with multiple exits leading to different destinations. These branches ensure that various regions of the face receive the appropriate sensory innervation. The auriculotemporal nerve, for example, provides sensation to the temple, while the lingual nerve supplies the tongue with sensory information.
Once the mandibular nerve reaches the mandible, it courses along the inferior alveolar canal—a canal located within the mandibular bone. This canal provides a protective pathway for the nerve and its associated blood vessels. Anterior to the mental foramen, the mandibular nerve changes its name and branches out into various smaller nerves, such as the mental nerve and incisive nerve.
The mental nerve, a branch of the mandibular nerve, innervates the lower lip, providing the ability to feel touch, temperature, and pain. It is responsible for the sensation you experience when you accidentally bite your lip or apply lipstick.
The incisive nerve, another branch of the mandibular nerve, supplies the lower teeth and gums with sensory innervation. This nerve allows us to perceive sensations such as pressure, temperature, and pain, enabling us to maintain oral health and seek appropriate dental care when needed.
As we explore the intricate details of the mandibular nerve, we gain a deeper appreciation for the complexity of our own anatomy. The mandibular nerve is not just a simple pathway for sensation; it is a vital component of our ability to experience and interact with the world around us.
The Mental Foramen: A Key Landmark in Dental Anatomy
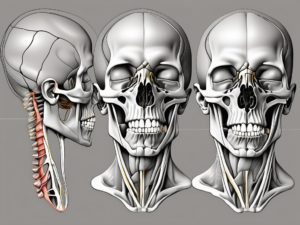
The mental foramen is a significant anatomical landmark in the mandible. Located on the anterolateral aspect of the mandible, it allows the mandibular nerve to exit the bone and provide sensory innervation to the tissues it supplies in the lower face.
The mental foramen is not just a simple opening in the mandible; it plays a crucial role in dental anatomy. Its precise location and function are of great importance to dentists and oral surgeons.
Location and Function of the Mental Foramen
The mental foramen is typically found between the lower premolars in the mandible. Its exact location may vary slightly among individuals, but it is usually situated in the premolar region, below the apex of the roots.
When examining a patient’s dental anatomy, dentists pay close attention to the mental foramen’s location. Its position can provide valuable information about the patient’s oral health and help determine the best treatment approach.
The mental foramen serves as a passageway for the mental nerve, a branch of the mandibular nerve responsible for innervating the lower lip, chin, and surrounding regions. This nerve is crucial for maintaining sensation and providing motor function to the lower face.
Without the mental foramen and the mandibular nerve, simple tasks like speaking, eating, and expressing emotions through facial expressions would be significantly impaired.
The Relationship Between the Mental Foramen and Mandibular Nerve
The mandibular nerve, after passing through the mental foramen, undergoes a transition from the inferior alveolar nerve to the mental nerve. This transition occurs at the level of the mental foramen, where the nerve changes its course and continues its sensory innervation in the lower face.
The intricate relationship between the mental foramen and the mandibular nerve highlights the complexity of dental anatomy. Dentists must have a deep understanding of this relationship to perform procedures such as nerve blocks, dental implants, and orthognathic surgeries.
During dental procedures, dentists must be cautious not to damage the mental nerve as it exits the mental foramen. Any injury to this nerve can lead to temporary or permanent numbness, tingling, or pain in the lower face, which can significantly impact a patient’s quality of life.
Furthermore, the mental foramen’s location and the mandibular nerve’s path can vary among individuals. Dentists must carefully assess each patient’s unique anatomy to ensure precise treatment planning and execution.
In conclusion, the mental foramen is a vital landmark in dental anatomy. Its location and function are crucial for maintaining sensation and motor function in the lower face. Dentists must have a thorough understanding of the relationship between the mental foramen and the mandibular nerve to provide safe and effective dental care.
The Mandibular Nerve Anterior to the Mental Foramen
Nomenclature and Identification
Anterior to the mental foramen, the mandibular nerve is referred to as the mental nerve or the incisive nerve, depending on the specific branches and regions it supplies. The mental nerve provides sensory innervation to the skin of the lower lip, chin, mucous membrane of the lower lip, vestibule of the lower lip, and the gum tissue in the premolar and anterior teeth region. The incisive nerve supplies sensory innervation to the anterior teeth and the associated mucous membranes.
Identifying and understanding the nomenclature of these nerve branches is crucial in dental practice, especially when administering local anesthesia, performing dental procedures, or assessing the causes of any sensory abnormalities in the lower face.
When it comes to the mental nerve, its name is derived from its location anterior to the mental foramen. This foramen is a small opening located on the mandible, specifically on the buccal surface. The mental nerve emerges from the mandibular canal, which is a tubular structure within the mandible that houses the inferior alveolar nerve. As the mental nerve exits the mental foramen, it branches out to provide sensory innervation to various structures in the lower face.
The incisive nerve, on the other hand, is responsible for supplying sensation to the anterior teeth and their associated mucous membranes. It is a branch of the mental nerve and travels anteriorly to reach the incisive foramen, which is located in the anterior region of the mandible. Through this foramen, the incisive nerve enters the oral cavity and distributes sensory fibers to the anterior teeth.
Clinical Significance of the Anterior Mandibular Nerve
Knowledge of the anatomy and function of the mandibular nerve anterior to the mental foramen is of utmost importance for dental professionals. Understanding the nerve’s course, landmarks, and variations helps in providing effective and safe dental treatments, such as nerve blocks and local anesthesia administration. Any damage or injury to the anterior mandibular nerve can lead to potential complications, including temporary or permanent sensory disturbances in the lower face.
During dental procedures, dentists and oral surgeons must exercise caution to avoid any inadvertent damage to the anterior mandibular nerve. This can be achieved through a thorough understanding of the nerve’s anatomical relationships and proper technique. By identifying the mental foramen and its associated nerves, dental professionals can accurately administer local anesthesia and perform nerve blocks to ensure patient comfort and successful treatment outcomes.
Furthermore, variations in the anatomy of the anterior mandibular nerve should be taken into consideration. While the mental nerve and incisive nerve follow a fairly predictable course, there may be instances where their paths deviate from the norm. These variations can occur in terms of the nerve’s position, size, or branching patterns. Therefore, dental professionals must be prepared to adapt their techniques and treatment plans accordingly to accommodate these anatomical differences.
In conclusion, a comprehensive understanding of the mandibular nerve anterior to the mental foramen is essential for dental professionals. By familiarizing themselves with the nomenclature, anatomy, and clinical significance of this nerve, they can provide optimal care to their patients, minimize the risk of complications, and ensure successful treatment outcomes.
Common Procedures Involving the Mandibular Nerve and Mental Foramen
Dental Procedures and the Mandibular Nerve
Various dental procedures necessitate an understanding of the relationship between the mandibular nerve and the mental foramen. These may include tooth extractions, dental implants, and periodontal surgeries involving the premolar and anterior tooth regions. Dentists need to carefully assess the position of the mental foramen, plan the surgical approach accordingly, and consider utilizing nerve-sparing techniques to prevent nerve injury.
When performing tooth extractions, dentists must be mindful of the mandibular nerve’s proximity to the roots of the teeth. The mental foramen, through which the mandibular nerve exits the mandible, is typically located near the apices of the premolar teeth. Dentists must exercise caution to avoid damaging the nerve during the extraction process, as injury to the mandibular nerve can lead to temporary or permanent numbness in the lower lip, chin, and tongue.
In dental implant procedures, the mandibular nerve’s position becomes even more critical. Dentists must carefully evaluate the location of the mental foramen to determine the appropriate placement of the implant. By utilizing advanced imaging techniques, such as cone beam computed tomography (CBCT), dentists can accurately map the course of the mandibular nerve and plan the implant surgery accordingly. This meticulous planning helps minimize the risk of nerve injury and ensures the long-term success of the dental implant.
Periodontal surgeries involving the premolar and anterior tooth regions also require a thorough understanding of the mandibular nerve’s anatomy. Dentists must consider the position of the mental foramen when performing procedures such as crown lengthening or gingival grafting. By carefully assessing the nerve’s location and taking necessary precautions, dental professionals can minimize the risk of nerve damage and optimize the outcomes of these periodontal surgeries.
Risks and Complications Associated with the Mandibular Nerve
Although dental procedures involving the mandibular nerve and mental foramen are generally safe, there are potential risks and complications to be aware of. Nerve injury, such as paresthesia or altered sensation, can occur if the nerve is damaged during a procedure. It is crucial for dental professionals to exercise caution, adhere to proper surgical techniques, and inform patients about the potential risks and benefits of any procedures involving the mandibular nerve.
During tooth extractions, the risk of nerve injury is always present. Dentists must carefully assess the position of the mental foramen and the proximity of the roots to the mandibular nerve. By employing gentle extraction techniques and considering nerve-sparing approaches, dentists can minimize the chances of nerve damage. However, in some cases, despite the utmost care, nerve injury may still occur, leading to temporary or permanent numbness in the lower lip, chin, and tongue. Dentists must inform patients about these potential risks and discuss the available treatment options in case of nerve injury.
In dental implant procedures, the risk of nerve injury is also a concern. Dentists must meticulously plan the surgery, taking into account the location of the mental foramen and the course of the mandibular nerve. By utilizing advanced imaging techniques and computer-guided implant placement, dentists can ensure precise implant positioning and minimize the risk of nerve damage. However, in rare instances, nerve injury may still occur, resulting in altered sensation or numbness. Dentists must educate patients about these potential complications and provide appropriate post-operative care to promote nerve healing and recovery.
Periodontal surgeries involving the premolar and anterior tooth regions also carry a risk of nerve injury. Dentists must exercise caution when performing procedures such as crown lengthening or gingival grafting, as the mental foramen’s proximity to these areas increases the likelihood of nerve damage. By employing meticulous surgical techniques and considering nerve-sparing approaches, dental professionals can reduce the risk of nerve injury. However, in some cases, nerve damage may still occur, leading to temporary or permanent sensory changes in the affected area. Dentists must inform patients about these potential complications and discuss the necessary precautions to minimize the risk of nerve injury.
Conclusion: The Importance of Understanding the Mandibular Nerve and Mental Foramen in Dental Practice
Mastering the anatomy, function, and clinical significance of the mandibular nerve and its relationship with the mental foramen is essential for dental professionals. By having a thorough understanding of these structures, dentists can make informed decisions, provide optimal treatments, and minimize the risks of complications. However, it is crucial to emphasize that patients should always consult with a qualified dental professional or healthcare provider for personalized advice and treatment options regarding their specific dental needs or concerns.