what kind of pain is there if the mandibular nerve is damaged
The mandibular nerve, also known as the inferior alveolar nerve, is a crucial component of the trigeminal nerve, the largest cranial nerve responsible for sensation in the face and motor functions of the jaw muscles. Damage to the mandibular nerve can result in various types of pain and discomfort, which can significantly impact an individual’s quality of life. This article aims to explore the different aspects of mandibular nerve damage, including its anatomy, causes, symptoms, diagnosis, treatment options, and living with the condition.
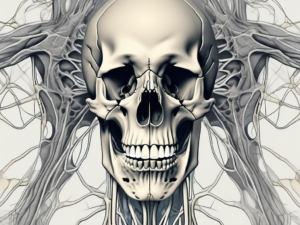
Understanding the Mandibular Nerve
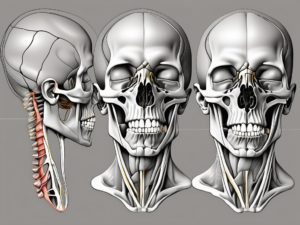
The mandibular nerve is one of the three main branches of the trigeminal nerve, originating from the trigeminal ganglion located within the skull. It travels through the infratemporal fossa and enters the mandibular foramen, providing sensory innervation to the lower jaw, lower teeth, lower lip, and part of the tongue. Additionally, it innervates the muscles responsible for chewing and biting, allowing us to perform vital functions such as eating and speaking.
The mandibular nerve is a fascinating component of the trigeminal nerve system. It plays a crucial role in our everyday lives, enabling us to experience sensations and perform essential actions like biting into a juicy apple or articulating words with precision.
As the mandibular nerve branches out from the trigeminal ganglion, it embarks on a remarkable journey through the infratemporal fossa. This anatomical pathway is a complex network of structures, including blood vessels, muscles, and connective tissues. The nerve navigates through this intricate terrain, ensuring that it reaches its destination—the mandibular foramen—where it can fulfill its sensory and motor functions.
Anatomy of the Mandibular Nerve
The mandibular nerve consists of both sensory and motor fibers. The sensory fibers transmit impulses related to touch, pain, and temperature, while the motor fibers control the movement and function of specific muscles in the jaw and face. This intricate combination of sensory and motor components allows the mandibular nerve to fulfill its multifaceted role in our daily lives.
Within the sensory fibers, there are specialized receptors that detect different types of stimuli. Some receptors are responsible for sensing light touch, allowing us to feel the gentle brush of a feather on our lower lip. Others are designed to detect pain, alerting us to potential harm and prompting us to take protective measures. The temperature receptors ensure that we can perceive hot and cold sensations accurately, helping us avoid burns or discomfort.
On the motor side, the mandibular nerve controls the muscles involved in chewing and biting. These muscles, known as the muscles of mastication, are essential for breaking down food into smaller, digestible pieces. Without the precise coordination provided by the mandibular nerve, our ability to chew and enjoy a variety of foods would be severely compromised.
Function of the Mandibular Nerve
The primary function of the mandibular nerve is to provide sensory feedback and motor control. Sensory signals from the lower face and oral cavity are transmitted through the mandibular nerve to the brain, allowing us to perceive sensations and respond accordingly. This feedback loop is crucial for our survival and well-being, as it enables us to detect potential dangers, such as a hot stove or a sharp object, and react swiftly to protect ourselves.
Motor impulses from the brain are relayed through the mandibular nerve to the muscles of mastication, facilitating the process of chewing, biting, and talking. These muscles work in harmony to grind and break down food, ensuring that it is prepared for digestion. The mandibular nerve acts as the conductor of this symphony of movements, ensuring that each muscle performs its role with precision.
Furthermore, the mandibular nerve also plays a role in the production of speech. It coordinates the movements of the tongue and lower lip, allowing us to articulate sounds and form words. Without the precise control provided by the mandibular nerve, our ability to communicate effectively would be significantly impaired.
In conclusion, the mandibular nerve is a remarkable component of the trigeminal nerve system. Its complex anatomy and innervation enable us to experience sensations, perform essential functions like chewing and biting, and communicate through speech. Understanding the intricacies of the mandibular nerve enhances our appreciation for the incredible mechanisms that enable us to navigate the world around us.
Causes of Mandibular Nerve Damage
The mandibular nerve can sustain damage due to various factors, including trauma, surgical complications, and dental issues. Understanding the potential causes can help individuals identify and address the underlying problem to minimize the impact on their nerve health.
Trauma and Injuries
Accidents, falls, or blows to the face can result in direct trauma to the mandibular nerve. Fractures of the mandible or other facial bones may cause compression, laceration, or stretching of the nerve, leading to potential damage. Additionally, damage can occur during dental procedures, particularly when extracting impacted wisdom teeth or performing corrective surgeries.
When it comes to accidents, the force of impact can be significant enough to cause damage to the mandibular nerve. For example, a person involved in a car accident may experience a direct blow to the face, resulting in trauma to the nerve. Similarly, athletes participating in contact sports like boxing or rugby are at a higher risk of sustaining injuries that can affect the mandibular nerve.
Fractures of the mandible, which is the lower jawbone, can also lead to mandibular nerve damage. These fractures can occur due to falls, physical altercations, or sports-related injuries. The broken bone may compress or lacerate the nerve, causing pain, numbness, or other symptoms.
Surgical Complications
Surgical interventions involving the lower jaw, such as orthognathic surgeries or temporomandibular joint procedures, pose a risk to the mandibular nerve. The close proximity of the nerve to the surgical site increases the likelihood of accidental nerve injury during these procedures.
Orthognathic surgeries, which are performed to correct jaw alignment issues, often require the repositioning of the lower jaw. During this process, the mandibular nerve can be inadvertently damaged, leading to potential complications. Similarly, temporomandibular joint procedures, which aim to address issues with the jaw joint, can also pose a risk to the mandibular nerve due to their proximity.
It is important to note that surgeons take precautions to minimize the risk of nerve damage during these procedures. However, due to the complex nature of the surgeries and individual anatomical variations, there is always a small possibility of nerve injury.
Dental Issues and Mandibular Nerve Damage
Dental infections, abscesses, or cysts in the lower jaw can put pressure on the mandibular nerve, causing compression and potential nerve damage. Prolonged dental issues, such as untreated cavities or gum disease, can also lead to nerve damage over time.
When dental infections or abscesses occur in the lower jaw, the swelling and inflammation can exert pressure on the mandibular nerve. This compression can impede the nerve’s function and cause pain, tingling, or numbness in the affected area. Similarly, cysts that develop near the mandibular nerve can also lead to nerve compression and potential damage if left untreated.
Untreated cavities or gum disease can have long-term consequences on oral health, including potential damage to the mandibular nerve. Cavities that are not addressed can progress and reach the inner layers of the tooth, potentially causing infection and inflammation in the surrounding tissues. Likewise, gum disease, if left untreated, can lead to the destruction of the supporting structures around the teeth, including the jawbone. This deterioration can affect the mandibular nerve and result in nerve damage.
Regular dental check-ups, proper oral hygiene practices, and timely treatment of dental issues are essential for maintaining oral health and minimizing the risk of mandibular nerve damage.
Symptoms of Mandibular Nerve Damage
The symptoms of mandibular nerve damage can vary depending on the extent and location of the injury. Common symptoms include:
Pain and Discomfort
Persistent or shooting pain in the lower jaw, teeth, and surrounding areas is a common symptom of mandibular nerve damage. The intensity may range from mild to severe, and it can be exacerbated by activities such as chewing or speaking.
In some cases, the pain may radiate to other areas of the face, causing additional discomfort. This can make it difficult for individuals to engage in daily activities and can have a significant impact on their quality of life.
It is important to note that the pain experienced may not always be constant. Some individuals may experience intermittent pain, while others may have a constant ache or throbbing sensation.
Sensory Changes
Alterations in sensation, such as numbness, tingling, or a “pins and needles” sensation, may occur in the lower lip, chin, gums, and tongue. This can lead to difficulties with feeling temperature, texture, or pain in the affected areas.
Individuals with mandibular nerve damage may find it challenging to enjoy certain foods due to the altered sensation in their mouth. They may struggle to differentiate between hot and cold temperatures, or they may have difficulty detecting the texture of certain foods.
In addition to the physical discomfort, these sensory changes can also have a psychological impact. Individuals may feel frustrated or anxious about their inability to fully experience the sensation of taste or touch in their mouth.
Speech and Eating Difficulties
Damage to the mandibular nerve can affect the movement of the muscles of mastication, leading to difficulties in chewing, biting, and speaking. Individuals may experience problems with proper articulation and pronunciation, as well as challenges in controlling food while eating.
These difficulties can significantly impact an individual’s ability to communicate effectively. They may struggle to pronounce certain sounds or words, leading to misunderstandings or difficulties in social interactions.
Furthermore, eating can become a challenging task for individuals with mandibular nerve damage. They may need to modify their diet to include softer foods that require less chewing, or they may require assistance in cutting food into smaller, more manageable pieces.
It is important for individuals experiencing these symptoms to seek medical attention. A healthcare professional can assess the extent of the nerve damage and develop a treatment plan to alleviate pain and improve function.
Diagnosing Mandibular Nerve Damage
Diagnosing mandibular nerve damage usually involves a comprehensive evaluation by a healthcare professional, such as a dentist or oral and maxillofacial surgeon. The diagnostic process typically includes:
Clinical Examination
The healthcare professional will conduct a thorough examination, assessing the patient’s dental and medical history, performing a physical examination of the affected areas, and discussing any symptoms experienced by the individual. They may also assess the patient’s motor and sensory function in the affected regions.
During the clinical examination, the healthcare professional will carefully inspect the patient’s oral cavity, looking for any signs of trauma or inflammation that may be indicative of nerve damage. They will also examine the patient’s teeth and gums, checking for any abnormalities or changes in sensation.
In addition to the physical examination, the healthcare professional will ask the patient about their symptoms, such as pain, numbness, or tingling in the jaw, lower lip, or chin. They will also inquire about any recent injuries or dental procedures that may have contributed to the nerve damage.
Imaging Techniques
Advanced imaging techniques, such as X-rays, computed tomography (CT) scans, or magnetic resonance imaging (MRI), may be utilized to visualize the structure of the affected jaw, teeth, and surrounding tissues. These imaging modalities can provide valuable insights into any potential nerve damage or structural abnormalities.
X-rays are commonly used to assess the alignment and position of the teeth, as well as the condition of the jawbone. They can help identify any fractures or dislocations that may have caused the mandibular nerve damage.
CT scans and MRI scans offer more detailed images of the oral and maxillofacial region. They can reveal the presence of tumors, cysts, or other abnormalities that may be compressing or impinging on the mandibular nerve. These imaging techniques can also help determine the extent of any nerve damage and guide treatment planning.
Nerve Conduction Studies
In some cases, nerve conduction studies may be recommended to assess the functionality of the mandibular nerve. This involves measuring the speed and strength of electrical impulses transmitted along the affected nerve, which can help determine the extent and nature of any nerve damage.
During a nerve conduction study, electrodes are placed on the skin overlying the mandibular nerve. Small electrical pulses are then delivered to stimulate the nerve, and the resulting electrical activity is recorded. By analyzing the speed and amplitude of the nerve impulses, healthcare professionals can evaluate the integrity of the mandibular nerve and identify any areas of dysfunction.
This diagnostic test can provide valuable information about the severity of the nerve damage and help guide treatment decisions. It can also help differentiate between nerve damage caused by trauma, infection, or other underlying conditions.
Treatment Options for Mandibular Nerve Damage
Treatment approaches for mandibular nerve damage primarily focus on managing symptoms, promoting nerve healing, and restoring optimal function. The choice of treatment depends on the underlying cause, severity of the damage, and individual patient factors. It is essential to consult with a healthcare professional to determine the most appropriate course of action.
Mandibular nerve damage can occur due to various reasons, such as trauma, infection, or nerve compression. The symptoms can range from mild discomfort to severe pain, numbness, and functional limitations. Prompt and proper treatment is crucial to prevent further complications and improve the quality of life for individuals affected by this condition.
Medication and Pain Management
Medications, such as non-steroidal anti-inflammatory drugs (NSAIDs) or analgesics, may be prescribed to manage pain and discomfort associated with mandibular nerve damage. These medications can help reduce inflammation, alleviate pain, and improve overall comfort. Additionally, nerve-specific medications, such as anticonvulsants or tricyclic antidepressants, may be recommended to alleviate neuropathic pain. These medications work by targeting the damaged nerve fibers and modulating the pain signals sent to the brain.
It is important to note that medication alone may not be sufficient to address the underlying cause of the nerve damage. Therefore, healthcare professionals often combine medication with other treatment modalities for a comprehensive approach to managing mandibular nerve damage.
Physical Therapy Approaches
Physical therapy techniques, including exercises and manual therapy, may be utilized to promote jaw muscle strength, improve range of motion, and facilitate nerve healing. Physical therapists with expertise in treating mandibular nerve damage can design personalized exercise programs to target specific muscle groups and improve overall jaw function.
In addition to exercises, manual therapy techniques, such as soft tissue mobilization and joint mobilization, can help reduce muscle tension, improve blood circulation, and enhance nerve regeneration. These therapies can also help individuals develop coping mechanisms to deal with pain, sensory changes, and functional difficulties. Physical therapy can play a significant role in the rehabilitation process, enabling individuals to regain optimal jaw function and improve their quality of life.
Surgical Interventions
In severe or complex cases of mandibular nerve damage, surgical interventions may be necessary. These procedures aim to repair or reconnect the damaged nerve, alleviate nerve compression, or address other underlying issues affecting nerve function. Surgical options should be thoroughly discussed with a healthcare professional, considering the potential risks and benefits.
One common surgical procedure for mandibular nerve damage is nerve grafting. This technique involves taking a healthy nerve from another part of the body, such as the leg, and using it to bridge the gap in the damaged nerve. Nerve grafting can help restore nerve function and promote healing in cases where the nerve damage is extensive or irreparable.
In some instances, nerve decompression surgery may be performed to relieve pressure on the damaged nerve. This procedure involves removing any structures or tissues that may be compressing the nerve, such as tumors or scar tissue. By alleviating the compression, the nerve can function more effectively, reducing pain and restoring normal sensation.
It is important to note that surgical interventions are typically considered when conservative treatments have failed to provide adequate relief or when the nerve damage is severe. The decision to undergo surgery should be made in consultation with a healthcare professional who can assess the individual’s specific condition and discuss the potential risks and benefits.
In conclusion, treatment options for mandibular nerve damage are diverse and depend on various factors. Medication and pain management, physical therapy approaches, and surgical interventions are some of the options available. A comprehensive approach that combines different modalities is often necessary to address the underlying cause, manage symptoms, and promote optimal healing and function. Consulting with a healthcare professional is crucial to determine the most appropriate treatment plan for individuals with mandibular nerve damage.
Living with Mandibular Nerve Damage
Coping with mandibular nerve damage can be challenging, both physically and emotionally. However, several strategies and resources can help individuals navigate their daily lives more effectively.
Coping Strategies
Managing chronic pain and sensory changes requires a multi-faceted approach. Utilizing relaxation techniques, engaging in stress-reducing activities, and maintaining a healthy lifestyle can contribute to improved overall well-being. Furthermore, exploring alternative therapies, such as acupuncture or mindfulness-based practices, may assist in managing symptoms.
Support and Resources
Seeking support from healthcare professionals, support groups, or online communities can provide valuable insights and guidance for individuals living with mandibular nerve damage. These resources can offer emotional support, information-sharing, and opportunities to learn from others who may have similar experiences.
Prognosis and Recovery
The prognosis for individuals with mandibular nerve damage varies depending on the extent of the injury, underlying cause, and individual factors. While complete nerve regeneration and recovery may not always be possible, many individuals experience improvements in symptoms over time with appropriate treatment and self-care practices. Consulting with a healthcare professional can provide personalized information regarding prognosis and recovery expectations.
In conclusion, damage to the mandibular nerve can result in various types of pain and discomfort, sensory changes, and functional difficulties. Understanding the anatomy, causes, symptoms, diagnosis, treatment options, and strategies for living with mandibular nerve damage is crucial for individuals affected by this condition. It is important to consult with a healthcare professional for proper evaluation, diagnosis, and guidance tailored to individual circumstances.