what muscles does the mandibular nerve innervate
The mandibular nerve is a crucial component of the trigeminal nerve, the fifth cranial nerve responsible for carrying sensory and motor information from the face to the brain. In this article, we will delve into the intricate details of the mandibular nerve, exploring its anatomy, functions, and its role in various muscular activities. Understanding the profound impact of the mandibular nerve on muscle control is essential for dental professionals and healthcare providers alike.
Understanding the Mandibular Nerve
Anatomy of the Mandibular Nerve
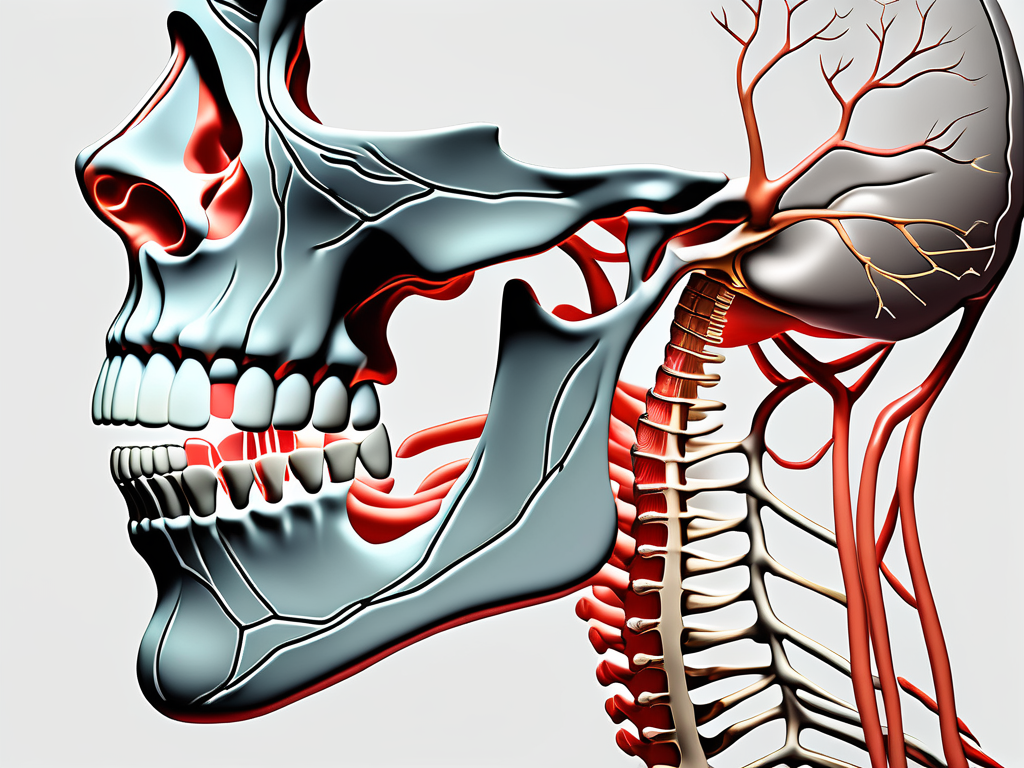
The mandibular nerve, also known as the third branch of the trigeminal nerve, emerges from the trigeminal ganglion located within the skull. It traverses through the foramen ovale, a bony opening in the skull, and branches into several divisions. This complex network of nerve fibers provides innervation to numerous muscles associated with mastication, facial expressions, and neck and throat movements.
The mandibular nerve is a remarkable structure that exhibits intricate anatomical features. As it emerges from the trigeminal ganglion, it is composed of both sensory and motor fibers, each serving a distinct purpose. The sensory fibers originate from the sensory ganglia, while the motor fibers arise from the motor nuclei within the brainstem.
Upon entering the foramen ovale, the mandibular nerve splits into multiple branches, each with its own specific function. One of the primary branches is the auriculotemporal nerve, which provides sensory innervation to the skin of the temple, external ear, and part of the scalp. This branch is responsible for transmitting sensations of touch, temperature, and pain from these areas.
Another important branch of the mandibular nerve is the inferior alveolar nerve. This branch descends into the mandible and provides sensory innervation to the lower teeth, gums, and lower lip. It plays a crucial role in oral perception, allowing individuals to sense pressure, temperature, and pain in the lower jaw region.
Function of the Mandibular Nerve
The mandibular nerve primarily serves a dual function, carrying both sensory and motor signals. Sensory fibers of the mandibular nerve provide tactile information from the skin of the lower face, lower lip, gums, and teeth. These sensations play a pivotal role in oral and facial perception.
On the other hand, the motor component of the mandibular nerve controls the movement of various muscles, allowing for crucial functions such as biting, chewing, swallowing, and even facial expressions. The harmonious interplay between the sensory and motor functions of the mandibular nerve is essential for maintaining optimal muscle control in the face and neck regions.
One of the significant motor branches of the mandibular nerve is the masseteric nerve. This branch innervates the masseter muscle, one of the primary muscles involved in the process of chewing. The coordinated contraction of the masseter muscle, facilitated by the mandibular nerve, allows individuals to effectively break down food into smaller, digestible pieces.
In addition to its role in mastication, the mandibular nerve also controls the movement of the temporalis muscle. The temporalis muscle is responsible for closing the jaw and plays a crucial role in biting and chewing. Without the proper innervation from the mandibular nerve, individuals would experience difficulties in performing these essential functions.
Furthermore, the mandibular nerve contributes to the innervation of the lateral pterygoid muscle, which is involved in jaw movement during chewing and swallowing. This muscle allows for lateral and protrusive movements of the mandible, enabling individuals to manipulate food within the oral cavity and facilitate the swallowing process.
The mandibular nerve also gives rise to the buccal nerve, which provides sensory innervation to the cheek and buccal mucosa. This branch allows individuals to perceive sensations such as touch, temperature, and pain in the cheek region, enhancing their overall oral and facial perception.
Overall, the mandibular nerve is a vital component of the trigeminal nerve system, playing a crucial role in both sensory and motor functions. Its intricate anatomy and diverse innervation patterns allow for the precise control of muscles involved in mastication, facial expressions, and neck and throat movements. Understanding the complexities of the mandibular nerve is essential for comprehending the intricate mechanisms underlying oral and facial perception, as well as the coordination of movements necessary for basic functions such as biting, chewing, and swallowing.
Muscles Innervated by the Mandibular Nerve
Masticatory Muscles
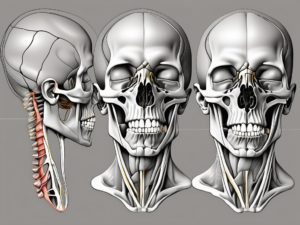
The mandibular nerve, a branch of the trigeminal nerve, innervates the masticatory muscles, which are responsible for the intricate movements involved in chewing and biting. These muscles include the temporalis, masseter, medial pterygoid, and lateral pterygoid muscles. Collectively, they coordinate to facilitate the precise and efficient grinding of food during mastication.
The temporalis muscle, located on the side of the head, is one of the key muscles involved in the chewing process. It is responsible for the elevation and retraction of the mandible, allowing for the powerful bite force required to break down food. The masseter muscle, located in the jaw area, is the primary muscle responsible for the closing of the jaw during chewing. It works in tandem with the temporalis muscle to generate the necessary force for effective mastication.
The medial pterygoid muscle, situated deep in the jaw, is responsible for the elevation and lateral movement of the mandible. It works in conjunction with the temporalis and masseter muscles to ensure smooth and coordinated chewing motions. The lateral pterygoid muscle, also located deep in the jaw, plays a crucial role in opening the jaw and moving it from side to side. This muscle is particularly important for tasks such as biting into larger food items or yawning.
Facial Expression Muscles
While the mandibular nerve is predominantly known for its involvement in masticatory muscle control, it also plays a significant role in regulating facial expressions. The muscles innervated by the mandibular nerve include the platysma, buccinator, and orbicularis oris muscles, among others. These muscles are instrumental in conveying emotions and enabling facial movements necessary for communication.
The platysma muscle, located in the neck region, is responsible for various facial expressions, such as frowning or tensing the neck. It plays a role in conveying emotions and can also assist in actions like opening the mouth wide. The buccinator muscle, situated in the cheek area, is responsible for compressing the cheeks during activities like blowing air or sucking. It also aids in keeping food between the teeth during chewing.
The orbicularis oris muscle, encircling the mouth, is crucial for various facial expressions, including smiling, puckering the lips, and speaking. It allows for precise control of the mouth’s opening and closing movements, facilitating clear articulation of speech sounds. These facial expression muscles, innervated by the mandibular nerve, contribute to the rich non-verbal communication that humans engage in on a daily basis.
Neck and Throat Muscles
Beyond the orofacial region, the mandibular nerve also supplies innervation to important neck and throat muscles. These muscles, such as the digastric, mylohyoid, and geniohyoid muscles, are essential for tasks like swallowing, speaking, and maintaining the stability of the hyoid bone. Precise control of these muscles is crucial for proper oral and pharyngeal function.
The digastric muscle, located in the neck, is responsible for elevating the hyoid bone during swallowing and speaking. It also assists in opening the mouth wide and stabilizing the hyoid bone during various movements. The mylohyoid muscle, forming the floor of the mouth, aids in elevating the hyoid bone and tongue during swallowing. It also plays a role in speech production, contributing to the clarity of certain sounds.
The geniohyoid muscle, situated in the neck region, is responsible for pulling the hyoid bone forward and upward during swallowing and speaking. It helps in maintaining the stability of the hyoid bone, which is crucial for proper functioning of the larynx and vocal cords. These neck and throat muscles, innervated by the mandibular nerve, work in harmony to ensure the smooth and efficient execution of essential tasks like swallowing and speaking.
Disorders Related to the Mandibular Nerve
Trigeminal Neuralgia
One of the most notable disorders associated with the mandibular nerve is trigeminal neuralgia. This condition causes severe facial pain, often described as electric shocks or stabbing sensations. Trigeminal neuralgia can significantly impact the quality of life, and individuals experiencing such symptoms are advised to consult a healthcare professional for proper diagnosis and management.
Trigeminal neuralgia is a chronic condition that affects the trigeminal nerve, which is responsible for transmitting sensory information from the face to the brain. The exact cause of trigeminal neuralgia is not fully understood, but it is believed to be related to compression or irritation of the trigeminal nerve.
The pain caused by trigeminal neuralgia can be triggered by various factors, including touching the face, chewing, speaking, or even a gentle breeze. The intensity and frequency of the pain episodes can vary from person to person, with some experiencing occasional mild pain and others enduring frequent and excruciating attacks.
Managing trigeminal neuralgia often involves a multidisciplinary approach. Medications such as anticonvulsants or muscle relaxants may be prescribed to help alleviate the pain. In some cases, surgical interventions may be necessary to relieve the compression or irritation of the trigeminal nerve.
Mandibular Nerve Palsy
Mandibular nerve palsy, a condition characterized by weakness or paralysis of the muscles innervated by the mandibular nerve, can result from various causes such as trauma, infections, or nerve damage during dental procedures. Consultation with a healthcare provider is crucial to determine the underlying cause and appropriate treatment options.
The mandibular nerve, also known as the inferior alveolar nerve, is a branch of the trigeminal nerve responsible for providing sensory and motor innervation to the lower jaw, lower teeth, and chin. When the mandibular nerve is affected, it can lead to difficulties in chewing, speaking, and controlling facial expressions.
Mandibular nerve palsy can occur due to trauma, such as a blow to the face or a fracture of the mandible. Infections, such as herpes zoster or bacterial infections, can also cause inflammation and damage to the nerve. Additionally, nerve damage during dental procedures, such as wisdom tooth extraction or dental implants, can result in mandibular nerve palsy.
Treatment for mandibular nerve palsy depends on the underlying cause and severity of the condition. In some cases, the nerve may recover on its own with time and rest. Physical therapy exercises may be recommended to help improve muscle strength and coordination. In more severe cases, surgical interventions or nerve grafts may be necessary to restore function to the affected muscles.
Treatment and Management of Mandibular Nerve Disorders
The treatment and management of mandibular nerve disorders vary depending on the specific condition and its severity. Healthcare professionals employ various approaches, including medication, non-surgical treatments, and surgical interventions, to alleviate symptoms and restore optimal nerve function.
Medication and Non-Surgical Treatments
For individuals experiencing mandibular nerve-related issues, medication may be prescribed to manage pain and reduce inflammation. Non-surgical interventions are also commonly recommended to alleviate symptoms and restore proper muscle function.
Physical therapy is often employed as a non-surgical treatment option. This approach involves exercises and techniques that aim to improve muscle strength, flexibility, and coordination. By targeting the affected muscles and nerves, physical therapy can help reduce pain and restore normal function.
In some cases, healthcare professionals may recommend nerve blocks as a means of pain management. Nerve blocks involve the injection of medication, such as a local anesthetic or a corticosteroid, into or near the affected nerve. This temporary numbing effect can provide relief from pain and allow for further therapeutic interventions.
Another non-surgical treatment option is the use of dental splints. These custom-made oral appliances are designed to reposition the jaw and provide support to the temporomandibular joint (TMJ). By stabilizing the jaw and reducing pressure on the mandibular nerve, dental splints can help alleviate pain and improve overall jaw function.
It is important to note that the appropriate treatment approach for mandibular nerve disorders may vary from person to person. Consulting with a healthcare professional, such as a neurologist or an oral and maxillofacial surgeon, is crucial in determining the most suitable treatment plan.
Surgical Interventions for Mandibular Nerve Disorders
In more severe or refractory cases, surgical interventions may be considered to address mandibular nerve disorders. These procedures aim to provide long-term relief and restore proper nerve function.
One surgical option is microvascular decompression (MVD). This procedure involves the placement of a small cushioning material between the affected nerve and the blood vessels that may be compressing it. By relieving the pressure on the nerve, MVD can alleviate symptoms and restore normal nerve function.
Nerve repair or grafting may be recommended in cases where the mandibular nerve has been damaged or severed. During this procedure, the damaged portion of the nerve is repaired or replaced with a graft, which can help restore nerve continuity and improve function.
In certain situations, neurectomy may be considered. Neurectomy involves the surgical removal of a portion of the affected nerve. This procedure is typically reserved for cases where other treatment options have been unsuccessful, and the nerve is deemed irreparable.
It is important to note that surgical interventions for mandibular nerve disorders should only be pursued after careful evaluation and discussion with healthcare specialists. The risks, benefits, and potential outcomes of each procedure should be thoroughly considered to ensure the best possible treatment outcome.
The Role of the Mandibular Nerve in Dentistry
Dental Procedures and the Mandibular Nerve
Given its close proximity to the mandibular nerve, dental professionals must exercise caution during various oral procedures. Local anesthesia techniques, such as inferior alveolar nerve blocks, aim to numb specific areas by temporarily blocking the transmission of nerve signals. Dentists with a deep understanding of the mandibular nerve’s innervation can ensure precise anesthesia administration and minimize the risk of nerve-related complications.
The mandibular nerve, also known as the inferior alveolar nerve, is a branch of the trigeminal nerve. It is responsible for providing sensory innervation to the lower teeth, gums, and lip on the same side of the face. This nerve plays a crucial role in dental procedures as it allows dentists to perform painless treatments, ensuring patient comfort and satisfaction.
During dental procedures, dentists must be mindful of the mandibular nerve’s location to avoid any accidental damage. The nerve runs through the mandibular canal, which is a bony canal located within the lower jaw. Any trauma or injury to this nerve can result in temporary or permanent numbness, tingling, or even loss of sensation in the affected area.
Mandibular Nerve Block Techniques
Mandibular nerve block techniques play a vital role in the field of dentistry, particularly in procedures involving the lower jaw. Techniques like the Gow-Gates technique or the Akinosi technique enable efficient and targeted anesthesia, optimizing patient comfort during dental treatments.
The Gow-Gates technique is a mandibular nerve block technique that involves injecting the anesthetic solution near the mandibular nerve trunk. By targeting the nerve trunk directly, this technique provides profound anesthesia to a larger area, making it suitable for extensive dental procedures such as extractions or implant placements.
On the other hand, the Akinosi technique is a mandibular nerve block technique that involves injecting the anesthetic solution into the pterygomandibular space. This technique is particularly useful when the patient has limited mouth opening, as it does not require wide mouth opening for administration. It provides effective anesthesia to the lower teeth and surrounding tissues, allowing dentists to perform various dental treatments with ease.
Both the Gow-Gates and Akinosi techniques require a thorough understanding of the mandibular nerve’s anatomy and precise injection placement. Dentists who are well-versed in these techniques can provide optimal pain control and ensure successful dental procedures.
Conclusion: The Importance of the Mandibular Nerve in Muscle Control
The complex innervation of the mandibular nerve allows for intricate muscle control involved in mastication, facial expressions, and other vital functions. Understanding the anatomy, functions, and disorders related to the mandibular nerve is of paramount importance for dental professionals, healthcare providers, and researchers alike.
While this article provides a comprehensive overview, it is crucial to remember that each individual’s condition can differ, and seeking professional advice is essential. Discussing any concerns or symptoms with a qualified healthcare professional will facilitate an accurate diagnosis and appropriate treatment plans, ensuring the best possible outcomes for individuals affected by mandibular nerve-related issues.