when does mandibular nerve become inferior alveolar
The mandibular nerve is a critical structure in the oral and facial region, responsible for innervating various muscles and transmitting sensory information. Understanding the anatomy and function of the mandibular nerve is crucial for dental and medical professionals alike. In this article, we will delve into the intricate details of the mandibular nerve’s transition into the inferior alveolar nerve, its role in the oral cavity, its relationship with other nerves, and potential problems that can arise.
Understanding the Anatomy of the Mandibular Nerve
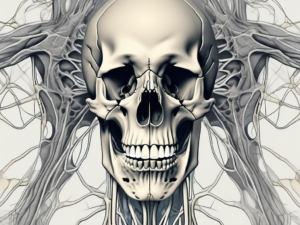
The mandibular nerve, also known as the V3 branch of the trigeminal nerve, is a fascinating structure that plays a crucial role in the functioning of the lower face and jaw. Let’s delve deeper into its intricate anatomy and functions.
The Structure of the Mandibular Nerve
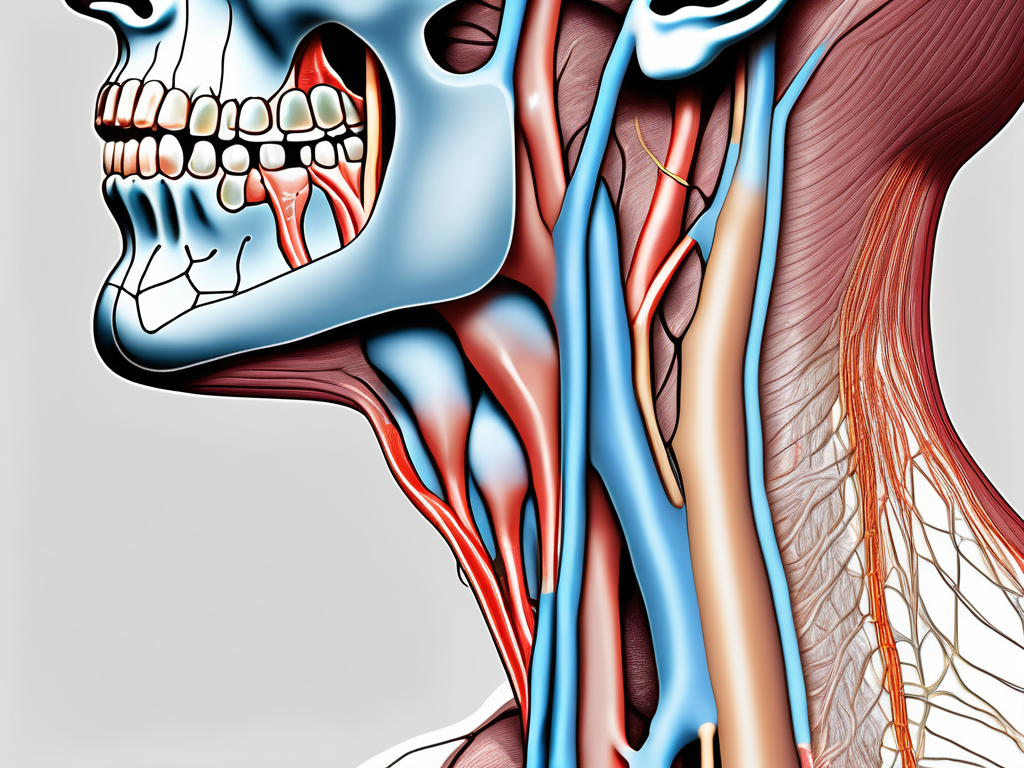
The journey of the mandibular nerve begins within the middle cranial fossa, where it emerges through the foramen ovale. This small opening allows the nerve to exit the skull and venture into the world outside. However, its course doesn’t end there.
Once outside the skull, the mandibular nerve splits into two primary branches: the anterior division and the posterior division. These branches take on different roles and supply various structures with the necessary innervation.
The anterior division is responsible for providing motor innervation to the muscles of mastication, which are vital for chewing and biting. These muscles include the temporalis, masseter, and pterygoid muscles. Additionally, the anterior division also provides sensory innervation to the lower teeth, lower lip, and chin region, allowing us to perceive sensations in these areas.
On the other hand, the posterior division of the mandibular nerve mainly carries sensory fibers. It supplies innervation to the skin of the cheeks, external ear, and temporomandibular joint. These sensory fibers play a crucial role in our ability to feel touch, temperature, and pain in these regions.
The Function of the Mandibular Nerve
While the anatomical structure of the mandibular nerve is fascinating, its functions are equally intriguing. Apart from its role in motor and sensory innervation, the mandibular nerve is involved in transmitting proprioceptive information.
Proprioception refers to our ability to perceive the position and movement of our body parts. In the case of the mandibular nerve, it allows us to have precise coordination during actions like biting and chewing. This proprioceptive information is crucial for the smooth functioning of our lower jaw and ensures that we can perform these actions accurately.
Furthermore, the mandibular nerve is also part of complex neural networks responsible for various reflexes. One such reflex is the jaw jerk reflex, which involves the rapid closure of the jaw in response to a tap on the chin. Understanding these intricate neural connections aids in the diagnosis and management of certain neurological conditions.
In conclusion, the mandibular nerve is a remarkable structure with a multifaceted role in the functioning of the lower face and jaw. Its anatomical complexity and diverse functions make it a subject of great interest and importance in the field of neuroscience.
The Transition of the Mandibular Nerve into the Inferior Alveolar Nerve
The Process of Transition
The transition of the mandibular nerve into the inferior alveolar nerve occurs within the infratemporal fossa, a deep space located in the posterior part of the maxillary tuberosity. This region is a complex and intricate network of structures, including muscles, blood vessels, and nerves. Within this intricate region, the mandibular nerve gives rise to the inferior alveolar nerve, which plays a key role in dental anesthesia and dental surgery procedures.
As the mandibular nerve travels through the infratemporal fossa, it reaches a critical point where it enters the mandibular foramen, a small opening in the mandible. This is the site where the transition takes place, and the mandibular nerve transforms into the inferior alveolar nerve. This transformation marks an important point in the nerve’s course, reflected in its change in nomenclature.
The inferior alveolar nerve, now formed from the mandibular nerve, continues its journey within the mandible, supplying sensation to the lower teeth, lower lip, and chin. It also sends branches to the mylohyoid muscle, which plays a role in the movement and stabilization of the mandible.
The Timing of Transition
The exact timing of this transition may vary among individuals. While the mandibular nerve generally becomes the inferior alveolar nerve at the level of the mandibular foramen, anatomical variations can occur, resulting in differing locations of transition. These variations can be influenced by factors such as the size and shape of the mandible, as well as individual differences in anatomy.
These anatomical deviations need to be considered in various dental procedures, such as inferior alveolar nerve blocks for local anesthesia. Dental professionals must have a thorough knowledge of these variations and anticipate potential challenges when administering local anesthesia. Failure to do so may compromise patient comfort and treatment outcomes.
Understanding the transition of the mandibular nerve into the inferior alveolar nerve is crucial for dental professionals. It allows them to accurately locate and target the nerve during dental procedures, ensuring effective anesthesia and successful treatment outcomes. By staying informed about the intricacies of this transition, dental professionals can provide optimal care to their patients and minimize the risk of complications.
The Role of the Inferior Alveolar Nerve
The Importance of the Inferior Alveolar Nerve
The inferior alveolar nerve, originating from the transition of the mandibular nerve, plays a significant role in oral health and function. It provides sensory innervation to the lower teeth and periodontium, conveying important tactile and nociceptive information to the central nervous system.
When it comes to dental procedures, the inferior alveolar nerve’s role cannot be overstated. Accurate clinical assessment of its function is crucial when planning and performing dental procedures, such as tooth extractions, implant placement, and periodontal surgeries. Dental professionals must have a deep understanding of the nerve’s anatomy and function to ensure successful outcomes.
Special care must be taken to avoid injury to this nerve during dental procedures. Any damage to the inferior alveolar nerve can lead to complications like altered sensation, paresthesia, or even permanent nerve damage. This highlights the importance of meticulous surgical techniques and the use of advanced imaging technologies to minimize the risk of nerve injury.
The Functions of the Inferior Alveolar Nerve
Beyond its sensory function, the inferior alveolar nerve also plays a crucial role in motor function. It transmits motor fibers to the mylohyoid muscle, a critical muscle involved in mandibular movement and stabilization. The mylohyoid muscle assists in actions like swallowing, speaking, and maintaining proper oral posture.
Understanding the role of the inferior alveolar nerve in both sensory and motor functions is essential for dental professionals. By comprehending its intricate functions, dental professionals can ensure optimal treatment outcomes and patient comfort. This knowledge allows them to tailor their treatment plans and techniques to minimize the risk of nerve damage while achieving the desired clinical goals.
Furthermore, advancements in dental technology have enabled more precise and accurate assessment of the inferior alveolar nerve’s function. Techniques such as nerve stimulation and intraoperative monitoring have revolutionized the field, allowing for real-time evaluation of nerve integrity during surgical procedures. These advancements have significantly improved patient safety and outcomes.
In conclusion, the inferior alveolar nerve is a vital component of oral health and function. Its sensory and motor functions make it indispensable in dental procedures and overall patient well-being. Dental professionals must prioritize the protection and preservation of this nerve to ensure successful treatment outcomes and minimize potential complications. Ongoing research and technological advancements continue to enhance our understanding of the inferior alveolar nerve, leading to improved clinical practices and patient care.
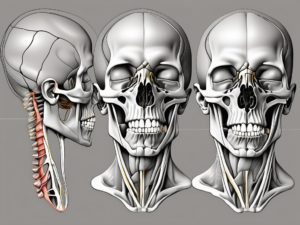
The Relationship between the Mandibular and Inferior Alveolar Nerves
The mandibular nerve and the inferior alveolar nerve share a close anatomical relationship. The mandibular nerve, also known as the V3 branch of the trigeminal nerve, gives rise to the inferior alveolar nerve through a process of transition within the infratemporal fossa.
The infratemporal fossa is a complex anatomical region located deep within the skull. It is bordered by various structures, including the zygomatic arch, the lateral pterygoid plate, and the temporal bone. Within this intricate network of bones and muscles, the mandibular nerve courses its way, eventually giving rise to the inferior alveolar nerve.
The inferior alveolar nerve, a branch of the mandibular nerve, is responsible for providing sensory innervation to the lower teeth, lower lip, and chin. It travels through the mandibular canal, a bony tunnel within the mandible, before branching out to supply these structures.
This interconnectedness highlights the importance of a comprehensive understanding of the mandibular nerve’s course and function in diagnosing and managing various oral and facial conditions. Knowledge of this relationship facilitates accurate diagnosis, appropriate treatment planning, and predictive outcomes.
The Impact of One Nerve on the Other
Disorders affecting the mandibular nerve can have secondary effects on the inferior alveolar nerve and vice versa. Conditions such as trigeminal neuralgia, a chronic pain disorder affecting the trigeminal nerve, can result in excruciating pain along the distribution of both the mandibular and inferior alveolar nerves.
Nerve compression, often caused by structural abnormalities or tumors, can also affect both nerves. When the mandibular nerve is compressed, it can lead to altered sensation or numbness in the lower teeth, lip, and chin supplied by the inferior alveolar nerve. Conversely, compression of the inferior alveolar nerve can cause referred pain or motor deficits in the muscles of mastication, which are innervated by the mandibular nerve.
Inflammation, such as that seen in conditions like temporomandibular joint disorder (TMJ), can also impact both nerves. Inflammatory processes can irritate the mandibular nerve, leading to pain and dysfunction in the muscles of mastication. This, in turn, can affect the function of the inferior alveolar nerve, resulting in altered sensation or pain in the lower teeth, lip, and chin.
It is crucial for healthcare professionals to identify the source of the problem accurately, as well as the potential involvement of both nerves, in order to provide appropriate interventions. Diagnostic testing, such as imaging studies and nerve conduction tests, may be necessary to establish an accurate diagnosis and develop an effective management plan.
Consultation with a specialist, such as a neurologist or oral and maxillofacial surgeon, may also be beneficial in cases where the relationship between the mandibular and inferior alveolar nerves is complex or when conservative treatments fail to provide relief. These specialists have the expertise to navigate the intricate anatomy of the nerves and offer targeted interventions, such as nerve blocks or surgical decompression, to alleviate symptoms and improve quality of life for patients.
Potential Problems and Disorders
The mandibular and inferior alveolar nerves are susceptible to various disorders that can significantly impact oral health and facial function. Understanding these disorders is crucial for dental professionals and healthcare providers involved in the management of these conditions.
Common Disorders of the Mandibular and Inferior Alveolar Nerves
Trigeminal neuralgia is one of the most prevalent disorders affecting the mandibular and inferior alveolar nerves. This condition is characterized by excruciating facial pain that can be triggered by simple activities such as eating or speaking. The pain often radiates along the mandibular division of the trigeminal nerve, causing significant discomfort and impairment in daily life.
Temporomandibular joint disorders (TMD) can also affect the mandibular and inferior alveolar nerves. TMD encompasses a range of conditions that affect the jaw joint and surrounding muscles. These disorders can cause pain, stiffness, and difficulty in opening or closing the mouth, leading to potential nerve compression or irritation.
In addition to trigeminal neuralgia and TMD, peripheral neuropathies can also impact the mandibular and inferior alveolar nerves. Peripheral neuropathy refers to damage or dysfunction of the peripheral nerves, which can result from various causes such as diabetes, infections, or autoimmune disorders. When these nerves are affected, individuals may experience numbness, tingling, or weakness in the lower face and jaw area.
Nerve injuries are another potential problem that can affect the mandibular and inferior alveolar nerves. These injuries can occur due to trauma, such as accidents or dental procedures, and can lead to temporary or permanent nerve damage. Nerve injuries can cause a range of symptoms, including pain, numbness, or loss of sensation in the affected area.
Treatment Options for Nerve Disorders
When it comes to treating nerve disorders involving the mandibular and inferior alveolar nerves, a comprehensive approach is essential. It is crucial to consult with a qualified healthcare professional or specialist to ensure accurate diagnosis and tailored management.
Medication is often the first line of treatment for nerve disorders. Depending on the specific condition, medications such as anticonvulsants, antidepressants, or pain relievers may be prescribed to alleviate symptoms and manage the underlying cause.
Nerve blocks are another treatment modality that can provide temporary relief from nerve-related pain. During a nerve block procedure, a local anesthetic is injected near the affected nerve to numb the area and interrupt pain signals. This can provide significant relief and allow individuals to engage in daily activities more comfortably.
Physical therapy may also be recommended as part of the treatment plan for nerve disorders. Physical therapists can design exercises and techniques to improve jaw mobility, reduce muscle tension, and promote overall oral and facial health. These exercises can help individuals regain function and alleviate pain associated with nerve disorders.
In severe cases or when conservative treatments fail to provide relief, surgical interventions may be necessary. Surgical options can range from nerve decompression to repair or reconstruction of damaged nerves. The choice of surgical intervention depends on the specific condition, severity of symptoms, and individual patient factors.
It is important to note that treatment options should be carefully considered and discussed with a qualified healthcare professional or specialist. The choice of treatment depends on factors such as the nature of the disorder, patient preferences, and potential long-term outcomes. A multidisciplinary approach involving neurologists, pain specialists, and dental professionals can ensure comprehensive and effective management of nerve disorders.
In conclusion, the mandibular and inferior alveolar nerves are vulnerable to various disorders that can significantly impact oral health and facial function. Understanding the complexities of these disorders and their treatment options is crucial for healthcare providers involved in the management of these conditions. By prioritizing accurate diagnosis, tailored management, and patient comfort, healthcare professionals can ensure optimal outcomes for individuals with potential problems and disorders affecting the mandibular and inferior alveolar nerves.