where is the mandibular nerve
The mandibular nerve, an essential component of the trigeminal nerve, plays a significant role in the sensory and motor functions of the face. Understanding the intricate anatomy and function of this nerve is crucial for healthcare professionals, particularly dentists, to ensure optimal patient care. In this article, we will delve into the depths of the mandibular nerve and explore its various aspects, ranging from its anatomical structure to its implications in dentistry.
Understanding the Mandibular Nerve
At its core, comprehending the mandibular nerve entails exploring its anatomical intricacies and understanding its multifaceted functionalities. The mandibular nerve, also known as the V3 division of the trigeminal nerve, is responsible for providing sensory innervation to the lower teeth, gums, lower lip, jaw, and tongue. Additionally, it plays a crucial role in motor functions such as chewing and biting.
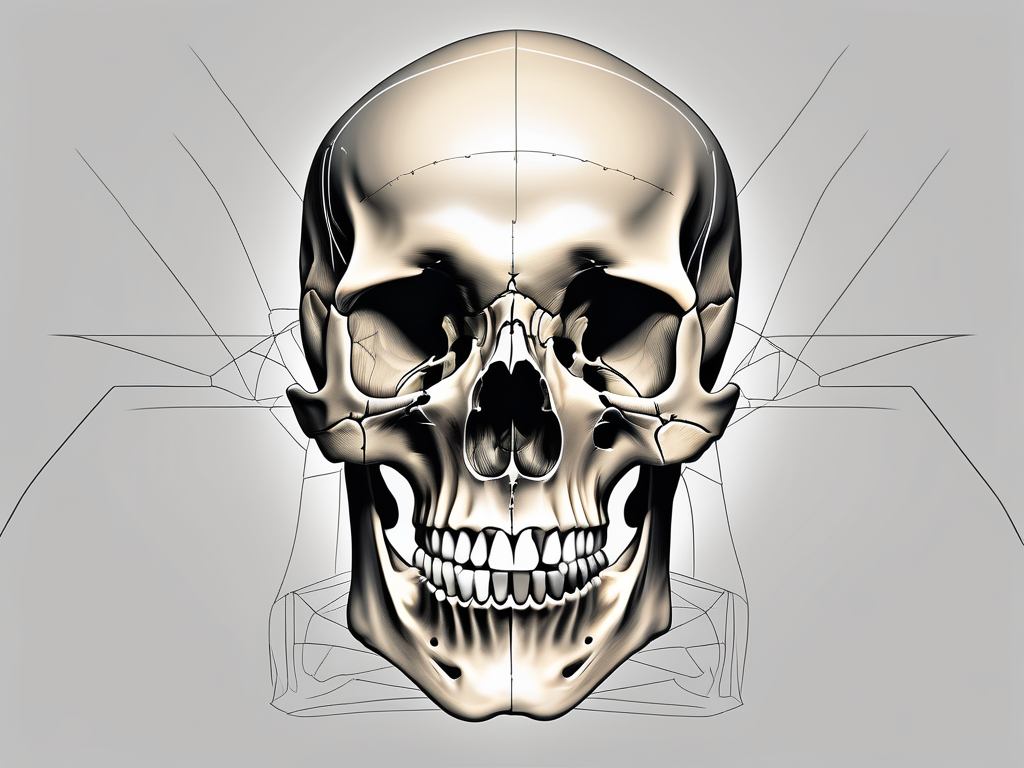
Anatomy of the Mandibular Nerve
The mandibular nerve originates from the trigeminal ganglion, located within the cranial cavity. This ganglion is a collection of nerve cell bodies that serves as a relay station for sensory information. After its inception, the nerve exits the skull through the foramen ovale, a bony structure positioned in the sphenoid bone. The foramen ovale acts as a gateway, allowing the mandibular nerve to extend its reach beyond the confines of the cranial cavity.
From there, the mandibular nerve traverses the infratemporal fossa, a region located below the temporal bone. This fossa is a complex anatomical space that houses various structures, including muscles, blood vessels, and nerves. As the mandibular nerve courses through this region, it gives off branches that supply sensory input to the various regions of the face mentioned earlier.
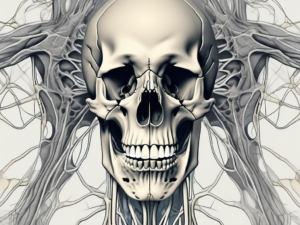
It is important to note that the mandibular nerve also gives rise to branches such as the buccal nerve and the lingual nerve, which are responsible for innervating specific areas within the oral cavity. The buccal nerve provides sensory innervation to the cheek and buccal mucosa, while the lingual nerve supplies sensation to the anterior two-thirds of the tongue.
Function of the Mandibular Nerve
The mandibular nerve serves as a vital conduit for both sensory and motor impulses. Sensory information from the lower face and oral cavity is transmitted via this nerve to the brain, enabling us to perceive touch, pain, and temperature. The sensory fibers within the mandibular nerve have specialized receptors that detect these stimuli and convert them into electrical signals that can be interpreted by the brain.
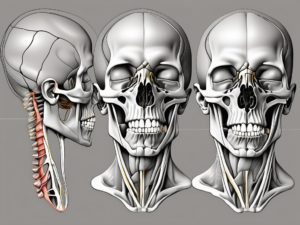
Furthermore, the motor branches of the mandibular nerve innervate the muscles responsible for mastication, facilitating crucial functions like biting and chewing. These muscles, including the masseter, temporalis, and medial pterygoid, work in harmony to generate the forces necessary for effective mastication. The mandibular nerve provides the necessary motor input to coordinate the contraction of these muscles, allowing for efficient chewing and biting.
Overall, the mandibular nerve is a complex and essential component of the trigeminal nerve system. Its intricate anatomy and multifunctional nature enable it to play a vital role in both sensory perception and motor control of the lower face and oral cavity. Understanding the intricacies of the mandibular nerve is crucial for healthcare professionals, as it allows for accurate diagnosis and treatment of various conditions affecting this region.
Locating the Mandibular Nerve
Locating the mandibular nerve is crucial for dental practitioners when administering anesthesia or performing intricate procedures. Understanding its position in the skull and its relationship to other facial nerves is imperative for successful interventions.
The mandibular nerve, also known as the V3 branch of the trigeminal nerve, is one of the three major divisions of the trigeminal nerve. It is responsible for providing sensory innervation to the lower teeth, lower lip, chin, and part of the tongue. Additionally, it controls the muscles involved in chewing.
Position in the Skull
The mandibular nerve can be found within the infratemporal fossa, a space located deep within the skull. This fossa is situated below the temporal bone and posterior to the maxilla. It is bounded by various structures, including the zygomatic arch, the lateral pterygoid plate, and the mandibular condyle.
Precisely identifying the location of the mandibular nerve allows clinicians to target the nerve effectively during nerve blocks or when delivering local anesthesia for dental procedures. By injecting the anesthetic agent near the nerve, dental professionals can provide pain relief and numbness to the areas innervated by the mandibular nerve. This precise administration ensures patient comfort and allows the dentist to carry out necessary treatments with ease and precision.
Relation to Other Facial Nerves
In addition to its anatomical positioning, understanding the relationship of the mandibular nerve to other facial nerves is crucial. The mandibular nerve shares proximity with branches of the facial nerve, particularly the buccal branches and the temporal branches.
The buccal branches of the facial nerve provide sensory innervation to the cheek and play a role in facial expression. They run in close proximity to the mandibular nerve, and it is essential to differentiate between the two to avoid inadvertent damage. Accidental injection of anesthetic agents into the buccal branches can lead to temporary facial paralysis or other complications.
The temporal branches of the facial nerve are responsible for innervating the muscles involved in raising the eyebrows and closing the eyelids. These branches also run in close proximity to the mandibular nerve. Careful consideration must be given to avoid any interference with the function of the facial nerve during dental procedures.
Identifying and distinguishing these nerves is important to prevent inadvertent damage and minimize potential complications. Dental practitioners undergo extensive training to develop the necessary skills and knowledge to navigate the intricate network of nerves in the face and ensure safe and effective treatment for their patients.
Disorders Related to the Mandibular Nerve
While the mandibular nerve’s function is vital for maintaining optimal dental health, certain disorders can compromise its normal functioning. Recognizing the symptoms of mandibular nerve disorders and being aware of available treatment options is essential for healthcare providers in managing such conditions.
The mandibular nerve, also known as the inferior alveolar nerve, is a branch of the trigeminal nerve responsible for providing sensory innervation to the lower teeth, lower lip, chin, and the mucous membranes of the mouth. It plays a crucial role in transmitting sensory information from these areas to the brain, allowing for normal oral function and sensation.
Mandibular nerve disorders can manifest in various ways, often leading to distressing symptoms for the affected individuals. These symptoms may include numbness or tingling sensations in the lower face, oral discomfort, difficulty in chewing or speaking, and persistent jaw pain. The intensity and frequency of these symptoms can vary depending on the underlying cause and individual factors.
One common disorder related to the mandibular nerve is trigeminal neuralgia, a condition characterized by severe facial pain. This pain can be triggered by simple activities such as eating, talking, or even touching the face. Trigeminal neuralgia can significantly impact a person’s quality of life, making it difficult to perform daily activities and causing emotional distress.
Another condition associated with the mandibular nerve is temporomandibular joint disorder (TMJ), which affects the joint connecting the jawbone to the skull. TMJ can cause pain, clicking or popping sounds when opening or closing the mouth, difficulty in fully opening the mouth, and even lockjaw in severe cases. It is often accompanied by muscle tension and headaches.
Consulting with a healthcare professional is paramount when experiencing any of these symptoms, as they can help identify the underlying cause and develop an appropriate treatment plan. A thorough medical history, physical examination, and diagnostic tests may be necessary to determine the exact nature of the mandibular nerve disorder and guide treatment decisions.
Treatment Options for Mandibular Nerve Disorders
Effective treatment of mandibular nerve disorders requires a comprehensive approach. Depending on the underlying cause, treatment options may include medication, physical therapy, nerve blocks, or, in severe cases, surgical intervention. Medications such as anticonvulsants and tricyclic antidepressants can help alleviate pain and reduce nerve sensitivity. Physical therapy techniques, including jaw exercises and relaxation exercises, can help improve jaw function and reduce muscle tension.
In some cases, nerve blocks may be recommended to provide temporary relief from pain. These blocks involve injecting an anesthetic or a combination of anesthetic and steroid directly into the affected area to numb the nerve and reduce inflammation. While nerve blocks can provide short-term relief, they are not a permanent solution and may need to be repeated periodically.
In severe cases where conservative treatments fail to provide relief, surgical intervention may be considered. Surgical options for mandibular nerve disorders include nerve decompression, where pressure on the nerve is relieved, and nerve repair or grafting, where damaged sections of the nerve are repaired or replaced with grafts. These procedures aim to restore normal nerve function and alleviate symptoms.
However, it is important to emphasize that each case is unique, and seeking professional advice from a qualified healthcare practitioner is essential in determining the most appropriate course of action. Treatment plans should be tailored to the individual’s specific needs, taking into account factors such as the severity of symptoms, underlying cause, and overall health status.
In conclusion, disorders related to the mandibular nerve can have a significant impact on oral health and overall well-being. Recognizing the symptoms and seeking timely medical attention is crucial for effective management. With advancements in diagnostic techniques and treatment options, healthcare providers can help individuals with mandibular nerve disorders regain normal function and improve their quality of life.
Importance of the Mandibular Nerve in Dentistry
The mandibular nerve, also known as the inferior alveolar nerve, plays a crucial role in dentistry beyond its general sensory and motor functions. Understanding the significance of this nerve is essential for dental professionals to ensure successful patient outcomes and provide optimal dental care.
The mandibular nerve is responsible for providing sensation to the lower teeth, gums, and lower lip. It also innervates the muscles involved in chewing, allowing for proper jaw movement and function. Without the proper functioning of the mandibular nerve, dental procedures can become challenging and may result in complications.
Role in Dental Procedures
During various dental procedures, such as extractions, root canals, or implant placements, a thorough understanding of the mandibular nerve’s location is paramount. Dental professionals must identify and respect the presence of this nerve to avoid potential nerve damage and its associated complications.
When performing extractions, dentists must carefully navigate around the mandibular nerve to prevent injury. By utilizing radiographic imaging and anatomical knowledge, they can determine the nerve’s proximity to the tooth being extracted and adjust their technique accordingly. Failure to do so can lead to nerve damage, resulting in altered sensation, persistent pain, or functional impairment of the lower face.
Root canal procedures also require precise knowledge of the mandibular nerve’s location. Dentists must ensure that the nerve is not inadvertently damaged during the removal of infected pulp from the tooth’s root canal system. By employing specialized instruments and techniques, dental professionals can effectively treat the tooth while minimizing the risk of nerve injury.
Implant placements in the mandible pose another challenge that highlights the importance of the mandibular nerve. Dental implants require careful placement in the jawbone to ensure stability and integration. Dentists must consider the position of the mandibular nerve to avoid damaging it during the implantation process. By utilizing advanced imaging techniques, such as cone-beam computed tomography (CBCT), dentists can accurately assess the nerve’s location and plan the implant placement accordingly.
Potential Risks and Complications
Despite careful planning and execution, there is always a potential risk of nerve injury during dental procedures involving the mandibular nerve. However, it is crucial to underline that the incidence of such injuries is relatively low when managed by experienced and skilled dental professionals.
Dental professionals undergo extensive training to develop the necessary skills and knowledge to mitigate the risks associated with mandibular nerve injury. By staying updated with the latest techniques and advancements in dental care, they can minimize the occurrence of complications.
In cases where the risks are considered higher, specialists, such as oral and maxillofacial surgeons, may be involved to ensure the utmost patient safety. These specialists possess advanced training and expertise in managing complex cases involving the mandibular nerve. Their involvement provides an additional layer of precaution, reducing the likelihood of nerve injury and its potential consequences.
Furthermore, advancements in technology, such as computer-guided surgery, have significantly improved the precision and safety of dental procedures involving the mandibular nerve. By utilizing computer-generated images and virtual planning, dentists can accurately assess the nerve’s position and plan the procedure accordingly, minimizing the risk of nerve injury.
In conclusion, the mandibular nerve plays a vital role in dentistry, particularly in dental procedures involving the lower jaw. Dental professionals must have a comprehensive understanding of the nerve’s location and take necessary precautions to avoid nerve damage. By prioritizing patient safety and utilizing advanced techniques, dentists can ensure successful outcomes and provide optimal dental care.
The Mandibular Nerve and Sensory Perception
The mandibular nerve not only plays a pivotal role in oral health and dental procedures but also significantly contributes to sensory perception within the face.
The mandibular nerve, also known as the inferior alveolar nerve, is a branch of the trigeminal nerve. It is responsible for providing sensory innervation to the lower teeth, gums, and lower lip. However, its impact goes beyond dental health.
Role in Taste and Touch
Sensory information related to taste and touch within the oral cavity passes through the mandibular nerve. This nerve carries signals from taste buds located on the tongue, allowing us to experience the wide range of flavors in our food. It also transmits touch sensations from the oral mucosa, enabling us to feel the texture, temperature, and consistency of what we eat.
Proper functioning of the mandibular nerve ensures the perception of various tastes and textures, significantly enhancing our enjoyment of food and facilitating the process of eating. It allows us to savor the sweetness of a ripe strawberry, the tanginess of a lemon, or the rich flavors of a well-prepared meal.
Impact on Speech and Eating
Mandibular nerve disorders can have adverse effects on speech and eating. When this nerve is compromised, patients may experience difficulty in articulating certain sounds or swallowing food adequately.
Speech difficulties can manifest as slurred or unclear speech, making it challenging for individuals to communicate effectively. Eating difficulties may include problems with chewing, biting, or moving food around the mouth, leading to discomfort and potential malnutrition.
Prompt identification and management of mandibular nerve disorders are crucial to mitigate these issues and improve overall quality of life. Dentists, oral surgeons, and neurologists work together to diagnose and treat conditions affecting the mandibular nerve, ensuring that patients can regain their ability to speak clearly and enjoy meals without discomfort.
In conclusion, the mandibular nerve is not only essential for oral health and dental procedures but also plays a vital role in sensory perception within the face. Its involvement in taste and touch allows us to experience the pleasures of food, while its impact on speech and eating highlights the importance of maintaining its proper function. By understanding the significance of the mandibular nerve, we can appreciate the complex interplay between our nerves, senses, and overall well-being.
Research and Advances in Mandibular Nerve Study
Advancements in medical and dental research continue to shed light on the intricacies of the mandibular nerve, uncovering new possibilities for improved diagnosis and treatment.
Recent Discoveries
Recent research has provided valuable insights into the anatomical variations of the mandibular nerve and its branches. Understanding these variations has the potential to enhance diagnostic accuracy and improve treatment outcomes, particularly in complex cases.
Future Implications for Medicine and Dentistry
The ongoing progress in mandibular nerve research holds promise for further advancements in medical and dental fields. Continued exploration may lead to novel therapeutic modalities, improved surgical techniques, and ultimately, enhanced patient care.
In conclusion, the mandibular nerve is a crucial component of the trigeminal nerve and plays a pivotal role in the sensory and motor functions of the face. Understanding its anatomy, function, and implications in dentistry is imperative for healthcare professionals, particularly dentists, to provide optimal care. By remaining vigilant of the potential risks and complications associated with the mandibular nerve and staying informed about recent advancements, dental practitioners can ensure safer and more effective treatment plans for their patients. Nevertheless, it is vital to consult with a healthcare professional for accurate diagnosis and personalized recommendations. Together, we can continue to unlock the mysteries of the mandibular nerve and advance the field of oral healthcare.